[Start here] NephMadness: Glomerulus Region – Podocyte Group
Meet the competitors for Glomerulus Region’s Podocyte Group!
Click here to view the entire Glomerulus Region.
Download complete NephMadness bracket in PDF or PPT
(1) Medicare kidney entitlement of 1972 vs (16) Transplant Chains
A true behemoth versus a diaper dandy. Glad to see transplant chains but this could be a difficult challenge.
Medicare kidney entitlement of 1972
In 1960 Belding Scribner working with Wayne Quinton invented a permanent and reusable vascular access device for intermittent hemodialysis, The first patient, Clyde Shields lived 11 years. Soon after that initial advancement small dialysis units began to spring up around the country but few patients were dialyzed. In 1972 the Congress was expanding the original Medicare bill to cover disabled people. As part of the testimony Shep Glazer received dialysis in front of the House Ways and Means Committee. He was attended by Georgetown nephrology fellow James Carey, In late December 1972 Section 299I passed granting medicare coverage for dialysis to all medicare eligible people in the United States (90% of the population). (See Rettig)
Transplant chains
Just over a year ago the New York Times published a story about a transplant chain that provided 30 patient with ESRD with kidney transplants. The chain began with Rick Ruzzamenti, an altruistic living donor, and ended with Donald Terry who had no friends or family members able to donate. The idea of allowing patients with a willing but incompatible donor to give their kidney to another person in the same situation was popularized in an article in the NEJM by Lainie Friedman Ross et al. in 1997. They attributed the idea to Rapaport in 1986. The first paired exchange was performed at Johns Hopkins in 2001. Hopkins also participated in the first multi-hospital complex chain involving 12 patients. In the US there are 90,000 people on the waiting list for a kidney. This system of facilitating living donors has the potential to move the needle and get lots of patients off dialysis who would otherwise just gaze at the unattainable spare kidneys of their loved ones.
(3) Fistula First vs (14) Peritoneal Dialysis First
Two initiatives to promote important topics in nephrology. Lets refresh ourselves.
Fistula First
The mortality of patients receiving dialysis in the United States is worse than many other countries. Numerous theories and explanations have been put forth to explain this gap but one fact that was always inescapable was the low rate of fistulas and high rate of AV grafts/catheters found in the US. In 2003 CMS, the ESRD Networks and other stakeholders initiated a National Vascular Access Improvement Initiative. The goal was to meet the current K/DOQI target of 50% incident patients and 40% prevalent patients using Fistulas. The program has been successful in moving patients from grafts to fistulas but the worst access of all, catheters, has not fallen, indicating additional work to be done. There is some data indicating that the increased focus on fistulas, with their finicky maturation rate, means that patients are relying on catheters for longer periods of time waiting for the fistula to mature. (See Lok Clin J Am Soc Nephrol. 2007;2:1043-53.)
Peritoneal Dialysis First
In the last 25 years peritoneal dialysis has fallen from representing about ~15% of the dialysis population to ~7%. This decrease in peritoneal dialysis use comes during a time when the modality is becoming safer, more convenient and more efficient. Consider:
- Less infections. Hemodialysis patients have 102 infections per 1000 patients years, PD patients have only 66.7 per 1000. (see USRDS 2011 Atlas, Figure 3.1)
- Home therapy. By allowing patients the opportunity to perform dialysis at home it gives them greater flexibility to manage their lives and continue working.
- Better transplant results. After transplant there is less delayed graft function, but that benefit may be balanced with other types of early graft loss. A more recent examination of the data found a small survival and graft benefit with PD.
- More cost effective. PD is $20,000 cheaper per year.
- Better satisfaction with care.
- It’s what nephrology professionals would choose if they needed dialysis.
A good summary of the peritoneal dialysis can be found here.
(12) K/DOQI vs (5) KDIGO
These are similar teams that should come down to the last seconds. Do I smell overtime?
K/DOQI
The kidney disease quality outcomes began in 1989 at a conference on in Dallas on excess morbidity in dialysis with a focus on dialysis dose. Following that conference a diverse group of stake holders banded together to produce clinical practice guidelines for the treatment of dialysis patients:
- Centers for Medicare and Medicaid Services [CMS]
- Association for the Advancement of Medical Instrumentation (AAMI)
- Renal Physicians Association (RPA)
- National Institutes of Health (NIH)
This crew, organized by the National Kidney Foundation, produced the Dialysis Outcomes Quality Initiative, DOQI guidelines. These guidelines published in 1997 called for:
- hematocrit of 33-36%
- spKt/V of at least 1.2
- URR of at least 65%
- Increase fistulas from 10 to 15% (compared to 50% elsewhere around the globe)
- Eliminate subclavian temporary catheters in favor of cuffed internal jugular catheters
By 2002 it was clear that DOQI was a success:
- Hematocrit rose from 30 to 34.5%
- URR rose from 63.8 to 69.9%
- Temporary catheters fell
- Permanent catheters rose
- Fistula rates increased
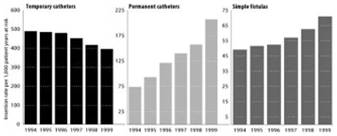
Fig 8 from 2002 KDOQI CKD. Insertion rates for central venous catheters and creation rates for simple fistulas per 1,000 patient-years at risk in US prevalent hemodialysis patients, 1994 to 1999.
DOQI shows that the U.S. dialysis apparatus was able to change practices and achieve goals laid out in clinical practice guidelines. Use of these guidelines was able to decrease variability of care from dialysis unit to dialysis unit and from doctor to doctor.
As the achievements of DOQI began to be actualized, it became clear to actually move the needle on dialysis outcomes the health of patients initiating dialysis would need to improve. This was the thinking behind targetting guidelines upstream and improving the health and performance status of people with the yet to be defined chronic kidney disease. The name for these expanded guidelines was Kidney Disease Outcome Quality Initiative, K/DOQI. The scope was bigger than dialysis, it would target the full range of chronic kidney disease from screening and diagnosis to dialysis and end of life issues.
In 2000 the first K/DOQI guidelines were published. They were updates of the four DOQI guidelines, it wasn’t until 2002 that the increased scope of K/DOQI was realized. In 2002 Spring Clinical meeting in Chicago The Chronic Kidney Disease: Evaluation, Classification, and Stratification guideline was released. This codified, for the first time, various levels of renal insufficiency, gave guidance on how to diagnose and screen for them and how to monitor these patients. This has ushered in a new era in nephrology.
KDIGO
Following the success of KDOQI other countries and other organizations assembled their own clinical practice guidelines. Naturally the guidelines varied in terms, targets, strength of evidence, and measuring techniques. To prevent an emerging tower of Babel and to minimize duplications of effort an international coalition was made to create an organization dedicated to:
“improve the care and outcomes of kidney disease patients worldwide through promoting coordination, collaboration and integration of initiatives to develop and implement clinical practice guidelines.”
KDIGO just published its CKD guidelines, the first revision of the initial CKD guidelines from 2002. One of the concerns about the initial guidelines was just how many people were diagnosed with CKD stage 3. Prior to automatic GFR reporting we had rampant underestimation of renal dysfunction as the frail and aged would escape notice with normal creatinines despite poor GFRs. After the CKD guidelines we had the reverse with vast populations getting caught in the GFR net due to normal aging and without structural or progressive renal failure. In 2007 Coresh et al. used NHANES data to project that 26 million Americans had CKD. To put this in perspective only 20 million Americans have diabetes. They projected that fully half of Americans over the age of 69 had CKD. A number of high profile editorials began to push back on the CKD definitions (see here and here).
KDIGO attempts to make this course correction by dividing the stage 3 into Stages 3A (GFR 45-59 ml/min) and 3B (GFR 30-44 ml/min) to grow the traditional 5 stages into 6 and then further risk stratifying patients by albuminuria:
- A1: < 30 mg/d
- A2: 30-300 mg/d
- A3: >300 mg/d
By combining the GFR and albuminuria stages into a 3×6 table they created a risk map to better judge prognosis. See the entire guideline at: http://www.kdigo.org/clinical_practice_guidelines/ckd.php
(10) DOPPS vs (7) USRDS
DOPPS
It is unfortunate but a reality that nephrology is based largely on retrospective data. We have only a few, mostly negative, randomized controlled trials, so our framework of care is largely based around retrospective observations and expert opinion. A large source of those observations comes from DOPPS.
The Dialysis Outcomes and Practice Patterns Study (DOPPS) comes out of the realization that outcomes differ from dialysis unit to dialysis unit and differences are even larger when you compare country to country. And behind those outcomes are different practices. Some of the variability may be due to different populations, comorbidities and genetic predispositions, but some of the variability is due to how dialysis is done. DOPPS’ mission is to mine those differences to determine which ones are translate into improved patient outcome.
DOPPS acts as the canary in the coal mine, able to quickly test theories and provide early guidance. It is not infallible and the organizers have not been dogmatic but looked to find where mistakes were made and improve the predictions for the future.
USRDS
The United States Renal Data Service is charged by congress to gather and track information on Medicare beneficiaries in the dialysis program. They also track patients not covered by medicare and provide the most complete data set on dialysis and transplant in the United States.
As part of the data distribution, USRDS publishes an Atlas of information regarding people with kidney disease. The Atlas does not look like any other government information I have ever seen. It is graphically rich and done with flourishes normally reserved for coffee table art books. Every year the Atlas has new design aesthetic. It is awesome:
Ready for the next group? Click here for Glomerulus, Mesangial Cell Group
Got bracket fever? Click here for the latest on Nephrology Madness!



PD first is my cinderalla. I say it goes deep. Maybe the Sweet 16!
Medicare Fistula First KDIGO USRDS – I’m just going by Popular/ity Vote