Test Your Knowledge: Interstitial Nephritis
In a recent article published in AJKD, Muriithi et al report a large series of 133 patients who had biopsy-proven acute interstitial nephritis at a single center. The following questions will test your pathology knowledge on this topic.
Post prepared by and all images courtesy of Tibor Nadasdy, MD, eAJKD Contributor and AJKD Kidney Biopsy Teaching Case Advisory Board member.
For a PDF version of the questions & answers, please click here.
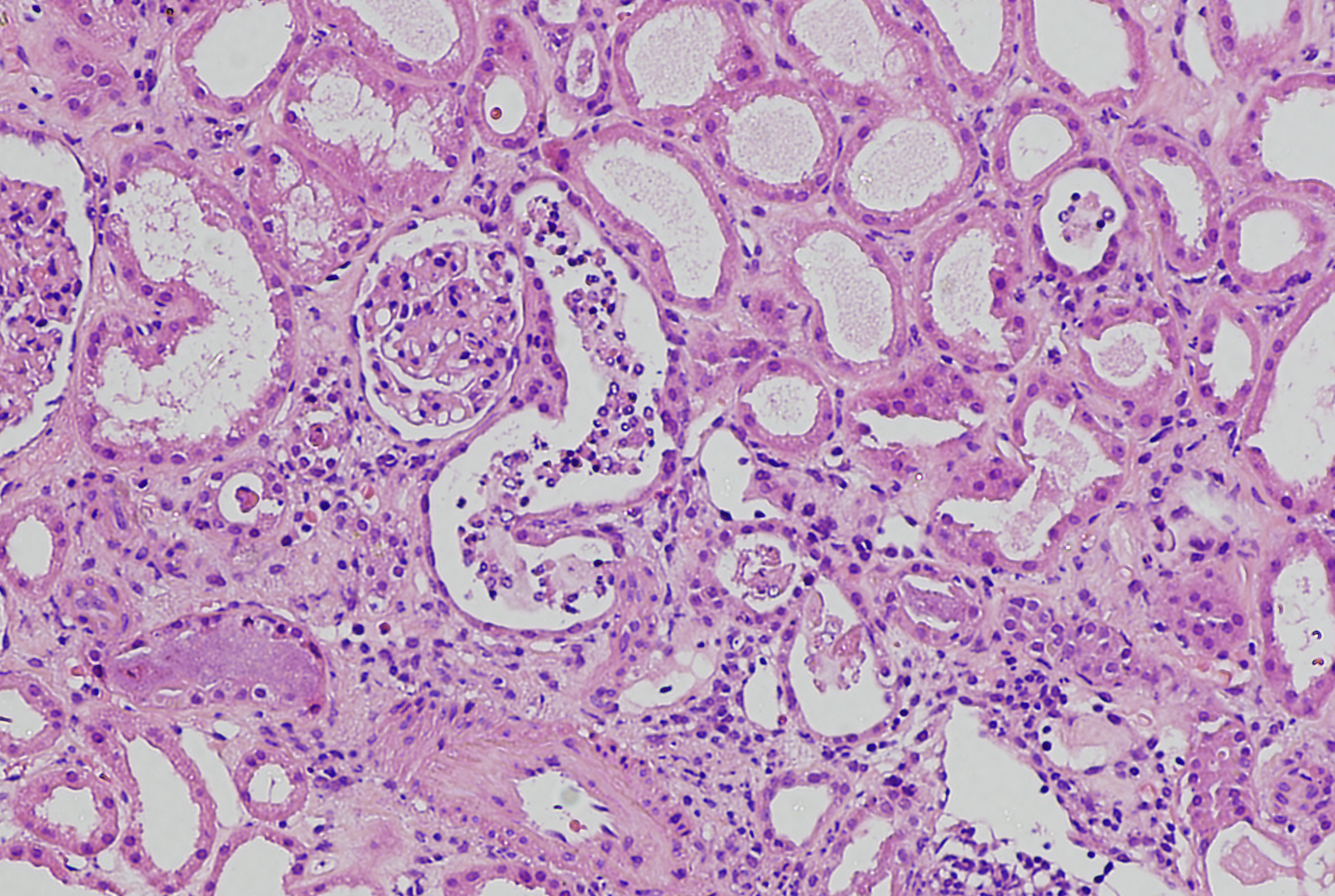
A 58-year-old woman with a history of ulcerative colitis was started on mesalazine three months before presentation. Previously, she had normal kidney function. She presented with fever, generalized symptoms, and an elevated serum creatinine of 3.7 mg/dL (eGFR, 13 mL/min by the CKD-EPI equation) that rapidly rose to 5.0 mg/dL (eGFR, 9 mL/min). Urinalysis showed numerous WBCs. She had no peripheral eosinophilia. Urine cultures indicated low numbers of Enterobacter and Candida. She had mild proteinuria on urinalysis and rare red blood cells in the urine sediment. Ultrasound imaging of the kidneys did not show abnormalities. A kidney biopsy was performed (image above). What is the most likely diagnosis?
Acute pyelonephritis evident by many polymorphonuclear leukocytes in the interstitium and tubules
Incorrect.
Autoimmune interstitial nephritis evident by mixed inflammatory cell infiltrate with many plasma cells
Incorrect.
Vasculitis-associated severe interstitial nephritis
Incorrect.
Severe drug-induced interstitial nephritis, probably secondary to mesalazine
Correct! Since the patient presented with fever, there were low numbers of Enterobacter and Candida in the urine, and the biopsy contained numerous polymorphonuclear leukocytes, the patient was initially treated with antibiotics after stopping mesalazine. No improvement was seen within the first week; therefore steroid treatment was started. Within a week into steroids, the patient’s kidney function improved and the patient regained normal kidney function.
Mesalazine is a rare cause of acute interstitial nephritis, but there are many cases published in the literature. In this particular patient, the main differential diagnosis was infection/acute pyelonephritis because she presented with fever and there were numerous polymorphonuclear leukocytes in the interstitium and renal tubules in the biopsy specimen. Polymorphonuclear leukocytes in the interstitium and tubules are characteristic of acute pyelonephritis; however, for acute pyelonephritis to cause such severe acute kidney injury, the disease has to be bilateral or associated with urosepsis. The presence of polymorphonuclear leukocytes in the interstitium and the tubules is not diagnostic of acute pyelonephritis. Polymorphonuclear leukocytes are common in severe forms of acute interstitial nephritis, including drug-induced interstitial nephritis. Clinical and morphologic signs of vasculitis or autoimmune disease were not evident.
A 63-year-old nondiabetic man developed an ischemic-appearing gangrenous toe on his foot. Because the lesions appeared infected, he was started on vancomycin and trough levels rose quickly above 50. He remained hemodynamically stable and his blood cultures were negative. His serum creatinine rose from 0.9 mg/dL (eGFR, 91 mL/min) to 2.7 mg/dL (eGFR, 24 mL/min). All his serologies were negative. Urinalysis showed no proteinuria or hematuria, but sediment evaluation revealed occasional granular casts and white blood cells. A kidney biopsy was performed (image above). The most likely diagnosis is:
ATN secondary to sepsis
Incorrect.
Acute tubular necrosis (ATN) and mild interstitial nephritis, probably secondary to vancomycin nephrotoxicity
Correct! The most likely explanation for the ATN and mild acute interstitial nephritis is high vancomycin levels. Vancomycin can be nephrotoxic, particularly in patients who have underlying chronic kidney disease. However, this patient who did not have pre-existing chronic kidney disease still developed ATN with mild interstitial nephritis. The constellation of ATN with mild interstitial nephritis is common in patients with vancomycin nephrotoxicity.
The diagnosis can be difficult because many times these patients are on a number of medications and also have numerous co-morbidities. However, after stopping vancomycin, this patient’s kidney function slowly started to normalize. The patient was not septic and had no risk factors for cholesterol embolization (he had gangrenous appearing toes but no livedo reticularis or any intervention that can lead to cholesterol emboli). He had peripheral vascular disease but remained hemodynamically stable.
ATN secondary to ischemia/peripheral vascular disease
Incorrect.
ATN secondary to cholesterol embolization
Incorrect.
A 44-year-old white man recently experienced bilateral parotid swelling and weight loss. His serum creatinine rose from 1.2 mg/dL (eGFR, 73 mL/min) to 3.1 mg/dL (eGFR, 23 mL/min) within three months. He has been taking NSAID. He was found to have bilateral hilar lymphadenopathy. Serum calcium level was slightly elevated at 10.8 mg/dL. Urine protein/creatinine ratio was 0.3. Urinalysis showed only 1-2 RBCs/HPF and 1+ protein. Other serologies, including ANA, ANCA, hepatitis B and C, are negative. Serum complement levels are normal. The most likely diagnosis is:
Lymphoma involving the salivary glands and kidneys
Incorrect.
Granulomatous interstitial nephritis secondary to sarcoidosis
Correct! This patient was diagnosed with sarcoidosis. He also underwent a lymph node biopsy, which showed nonnecrotizing granulomatous lymphadenitis. He was started on steroids, which were then tapered off. His serum creatinine decreased to 1.3 mg/dL (eGFR, 66 mL/min) within six months after the diagnosis.
Granulomatous interstitial nephritis is characteristic in sarcoidosis; however, the granulomas may be missed in a small biopsy specimen. Granulomatous interstitial nephritis can be seen in a variety of other conditions, including drug-induced interstitial nephritis, rare infections (such as tuberculosis or brucellosis), granulomatous vasculitis, and occasionally without an underlying etiology (idiopathic granulomatous interstitial nephritis). In this patient, there was no evidence of vasculitis or infection. Lymphomas do not cause granulomatous interstitial nephritis and steroid treatment alone would not help. NSAID-induced granulomatous interstitial nephritis is a theoretical possibility, but much less likely than sarcoidosis given the clinical history.
Granulomatous vasculitis
Incorrect.
Interstitial nephritis secondary to NSAID use
Incorrect.
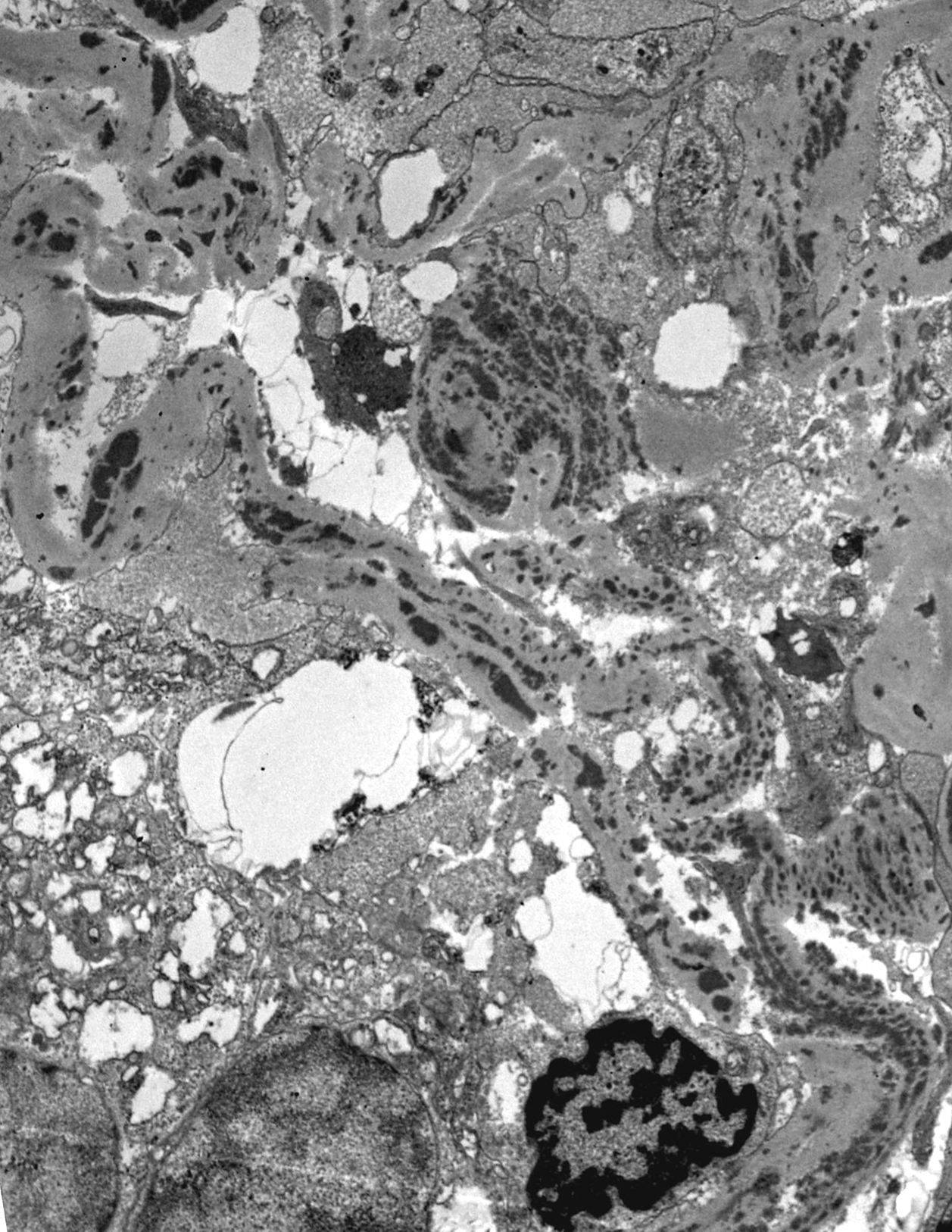
An 83-year-old man with a history of type II diabetes and chronic kidney disease was found to have progressive worsening of his kidney function; his serum creatinine rose from 2.1 mg/dL (eGFR, 28 mL/min) to 6.3 mg/dL (eGFR, 7 mL/min) in an eight-month period. Urine protein/creatinine ratios ranged from 0.6 to 0.8. Urinalysis shows 1+ protein and trace blood. ANA was positive at 1:640, ANCA was negative, C3 and C4 low at 71 and 9, respectively, and SPEP and UPEP negative for monoclonal spike. A kidney biopsy was performed with the images showing representative light microscopy, immunofluorescence (IgG), and electron microscopy (a tubule) images. The most likely diagnosis is:
IgG4-related interstitial nephritis
Correct! This patient has IgG4-related interstitial nephritis. The renal parenchyma is involved by a heavy plasma-cell-rich interstitial inflammatory cell infiltrates associated with variable degree of fibrosis. Large numbers of the plasma cells (over 50 plasma cells/HPF) were IgG4 positive by immunoperoxidase stain. IgG-containing tubular basement membrane deposits were abundant by immunofluorescence, and electron microscopy confirmed the presence of electron dense immune type deposits in the tubular basement membranes. IgG4-related interstitial nephritis frequently has a zonal distribution forming bulky tumor-like masses in the kidney. Fortunately, the disease is usually steroid responsive.
In lupus nephritis, IgG-containing deposits along the tubular basement membranes are not unusual; however, the interstitial plasma cells are not IgG4 dominant. Also, such bulky plasma-cell-rich interstitial inflammatory cell infiltrates are unusual in lupus nephritis. Drug-induced interstitial nephritis rarely has so many plasma cells, and tubular basement membrane deposits are absent. Although there was prominent chronic injury in the biopsy, the active plasma-cell-rich inflammation and the tubular immune complex deposits are not characteristic findings in advanced stage diabetic nephropathy.
Lupus nephritis with prominent interstitial inflammatory cell infiltrate
Incorrect.
Drug-induced interstitial nephritis
Incorrect.
End-stage diabetic nephropathy
Incorrect.





Leave a Reply