NephMadness 2016: Hypertension Region
Submit your picks! | For more on NephMadness 2016 | #NephMadness or #HTNRegion on Twitter
Since Guyton discovered the infinite feedback gain property of the kidney-fluid mechanism for pressure regulation, the fields of nephrology and hypertension have been intimately linked. Despite the primacy of the kidney in maintaining blood pressure and even causing high blood pressure, how much does high blood pressure damage the kidneys, compared to its well established role in causing stroke and heart failure?
Renal sympathetic denervation almost brought hypertension within the renal sphere of influence, though it proved to be a false start. But now, recent research is making hypertension cool and controversial again. The biggest story of 2015 was the release of the SPRINT data which reported a reduction in all-cause mortality with a more intensive (<120 mm Hg) blood pressure target (see #NephJC discussion here). Whether this will lead to an about turn in the major hypertension guidelines (including the NephMadness 2014 champion, JNC8) is something that will play out in the next few months.
Accurate blood pressure measurement is crucial to the diagnosis and treatment of hypertension. The multiple steps needed and the time and diligence required, however, means that office blood pressure are often measured poorly. Ambulatory blood pressure monitoring (ABPM) was established as a “gold standard” for measurement of blood pressure. We will examine how and why this came to be. More recently, automated oscillometric blood pressure monitoring has come in vogue, and was even used in the recently released SPRINT trial. Can this upstart replace ABPM?
Selection Committee member for the Hypertension Region:
Dr. Raymond Townsend
Dr. Townsend is a Professor of Medicine at Penn and an Associate Director of the CTSA at Penn. His research is in BP related mechanisms like vascular stiffness and pulse wave analysis and how these influence CKD progression, and CVD in CKD patients. He is a SPRINT investigator, a battered survivor of the JNC 8 panel, and he makes a wicked sausage lasagna.
Meet the Competitors for the Hypertension Region
Ambulatory BP
SPRINT BP Monitoring
BP for CKD vs BP for CVD
Introduction: Lowering Blood Pressure decreases Kidney Disease
Do bad kidneys cause high blood pressure?
or
Does high blood pressure cause bad kidneys?
Rather than the “does the chicken or the egg comes first” analogy, high blood pressure and kidney disease should be thought of as an interlinked vicious cycle, which feed each other and make things mutually and progressively worse. After all, both the NIDDK and the American Heart Association agree on the risk that high blood pressure poses to the kidneys, and the importance of blood pressure control for protecting the kidneys.
Blood pressure for CKD
 In study after study we see that achieved blood pressure correlates with progression of renal failure. Even in studies that fail to show that lower blood pressures results in decreased progression of renal failure when you organize the results by achieved blood pressure rather than by intention to treat we see that lower blood pressures have slower progression of renal failure. Look at the MDRD trial: 840 patients randomized to usual blood pressure or lower blood pressure. The primary study did not show an effect of lowering the blood pressure on development of ESRD, but when you look at achieved blood pressure, patients with more than a gram of proteinuria (most of the patients in MDRD), lower blood pressure resulted in better outcomes.
In study after study we see that achieved blood pressure correlates with progression of renal failure. Even in studies that fail to show that lower blood pressures results in decreased progression of renal failure when you organize the results by achieved blood pressure rather than by intention to treat we see that lower blood pressures have slower progression of renal failure. Look at the MDRD trial: 840 patients randomized to usual blood pressure or lower blood pressure. The primary study did not show an effect of lowering the blood pressure on development of ESRD, but when you look at achieved blood pressure, patients with more than a gram of proteinuria (most of the patients in MDRD), lower blood pressure resulted in better outcomes.
A post hoc analysis of the positive RENAAL study (which demonstrated the renoprotective effect of losartan in type 2 diabetic nephropathy) shows the predictive power of hypertension. A systolic blood pressure (SBP) at the start of the trial of 140-159 mm Hg increased the risk of developing ESRD by 37% compared to a SBP less than 130 mm Hg. If the SBP was over 160, it doubled the risk of ESRD compared to a systolic of 130. The same analysis also looked at achieved blood pressure (with losartan compared to placebo), the risk of ESRD was lower with an achieved blood pressure of below 140/90 compared to higher blood pressure.
Even an analysis from the negative ONTARGET trial of dual-renin-angiotensin system blockade (ramipril + telmisartan) reported that renal outcomes were less likely with lower achieved blood pressure. Lastly, a systematic review and meta-analysis examined the specific question of renal protection with more intensive blood pressure targets in RCTs with more than 6-month follow up. With a pooled analysis including 9287 patients from 11 trials with 1264 kidney failure events, there was a significant decrease in the risk of ESRD (HR 0.79, 95% CI 0.67-0.93).
These examples do not stand alone, in trial after trial one can see a clear association with high blood pressures and higher progression of renal failure. Bakris et al collected this data in this graph that showed a linear association between mean arterial pressure and progression of renal failure.

Figure 1. Relationship between achieved blood pressure control and declines in GFR in clinical trials of diabetic and nondiabetic renal disease. In the table, the trials marked by an asterisk are those in nondiabetic renal disease patients. Reproduced from Bakris et al, used with permission.
The trial to take a look at is the HALT-PKD study which looked at total kidney volume (a robust surrogate of progression) in 558 polycystic kidney disease patients who were randomized to a lower blood pressure target (95 to 110 mm Hg) compared to typical blood pressure target. This study stands alone in showing an improved kidney outcome (though admittedly a surrogate outcome) in an ITT analysis from lower blood pressures.
Conclusion
BP control is the cornerstone of risk reduction in the management of the CKD because in study after study, patients with the lower blood pressure have slower progression to renal failure.
Blood pressure control lowers cardiovascular disease, not kidney disease
 Blood pressure is tightly linked to cardiovascular disease, particularly stroke, as graphically represented by FDR’s blood pressure (see Figure 1 in Bishop & Figueredo ).
Blood pressure is tightly linked to cardiovascular disease, particularly stroke, as graphically represented by FDR’s blood pressure (see Figure 1 in Bishop & Figueredo ).
A few years later, in 1967, the Veterans Affairs Cooperative group reported a dramatic reductions (27 versus 2) in severe, complicating, events with blood pressure treatment in 149 men with diastolic BP over 115 mmHg (think about that, you send patients to the ER with diastolics of 115, in 1967 they were sending them to be randomized to blood pressure control or placebo). Over the years, blood pressure targets have steadily fallen as the data and our comfort with treatment has increased. The latest example is the SPRINT trial, which showed a remarkable decrease in cardiovascular outcomes with intensive blood pressure lowering (HR 0.75, 95% CI 0.64 to 0.89) and a NNT of only 60 over 3.7 years. A subsequent meta-analysis (123 studies, 613,815 participants) reports that a 10 mm Hg decrease in SBP leads to a 13% decrease in all cause mortality, along with reductions in stroke, heart failure, and coronary events.
Blood pressure control does not lower chronic kidney disease outcomes
The MDRD trial and the AASK trial results are often quoted as support for a lower blood pressure target to lower CKD outcomes, in CKD patients especially those with proteinuria. However, the benefit of blood pressure lowering reported in both of these trials is from post hoc analysis of a subgroup that was not pre-specified. Such analyses can just as often reflect a coincidental finding rather than a truth. We should consider these findings as merely hypothesis generating and in need of replication in subsequent trials.
The AASK analysis uses achieved blood pressure in a study where the intention-to-treat analysis was negative. This means that prescribing a lower blood pressure did not benefit patients, but patients that happened to achieve the lowest blood pressures did well. This suggests that other factors besides the lowering the blood pressures were responsible for the benefit. This post-hoc finding could be due to better baseline kidney function, less significant comorbidities, less alcohol, lack of smoking, etc. This kind of analysis is very susceptible to confounding and should be viewed with a jaundiced eye.
REIN-2 (N=338) was a trial specifically done to test intensive blood pressure lowering in patients with proteinuric CKD, and failed to show any benefit (HR 1.00, 95% CI 0.61 to 1.64). If one needs more convincing, the recent SPRINT trial—which showed a remarkable risk reduction in all-cause and cardiovascular mortality—is quite revealing. Among the 2,646 patients with CKD at baseline, there was no benefit with intensive BP control for any renal outcome (need for dialysis, transplant, doubling of creatinine, incident albuminuria). Among those without CKD at baseline, there an increased risk of their FR falling by 30% (HR 3.49, 95% CI 2.44 to 5.10).
Two other trials that are worth mentioning are two that looked at dual renin-angiotensin system blockade. The ONTARGET trial (with ramipril and telmisartan) which looked at patients with elevated CV risk but without CKD did not show any benefit in clinical outcomes, and even showed an increase in acute kidney injury with dual RAS blockade. The VA-NEPHRON-D trial, that looked at patients with diabetic kidney disease, also showed an increase in acute kidney injury and hyperkalemia dual RAS blockade. These two trials did, however, demonstrate, a reduction in proteinuria. Thus, a reduction in proteinuria was not accompanied by a reduction in meaningful clinical outcomes, and with had an increase in acute kidney injury. To complete the picture, the systematic review quoted above from The Lancet last month reports that despite the impressive reduction in cardiovascular events, the decrease in renal failure is not significant (HR 0.95, 95% CI 0.84 to 1.07).
Conclusion
Blood pressure reduction is a laudable goal, and should be pursued diligently and doggedly. It reduces cardiovascular events and mortality. But let us not harbour any illusions that it reduces kidney failure. This does not mean that we should let therapeutic nihilism overcome us when treating CKD patients—blood pressure reduction in these patients does help reduce cardiovascular events—and will keep them alive longer.
Ambulatory BP vs SPRINT BP Monitoring
Ambulatory Blood Pressure Monitoring
 One of the first descriptions of ambulatory blood pressure monitoring was from John Floras and the Oxford group, who demonstrated the differential effects of different beta-blockers on 24-hour blood pressure using invasive, intra-arterial blood pressure measurement. Non-invasive ambulatory blood pressure monitoring (ABPM) on a large scale was first described by Perloff and Sokolow in 1983, but it was Thomas Pickering who played a key role in the subsequent research and popularization of this technique (read this for a fascinating description of the life and research of Thomas Pickering). Along with John Laragh, Pickering described ABPM as a way to gather more clinical information for “borderline” hypertensives, then described as diastolic blood pressure ≤95. Laragh and Pickering were able to show that most of these patients were not hypertensive outside of the physician’s office, foreshadowing the description of “white coat” hypertension. They also discovered masked hypertension and nocturnal dipping. The three main advantages of performing an ABPM are:
One of the first descriptions of ambulatory blood pressure monitoring was from John Floras and the Oxford group, who demonstrated the differential effects of different beta-blockers on 24-hour blood pressure using invasive, intra-arterial blood pressure measurement. Non-invasive ambulatory blood pressure monitoring (ABPM) on a large scale was first described by Perloff and Sokolow in 1983, but it was Thomas Pickering who played a key role in the subsequent research and popularization of this technique (read this for a fascinating description of the life and research of Thomas Pickering). Along with John Laragh, Pickering described ABPM as a way to gather more clinical information for “borderline” hypertensives, then described as diastolic blood pressure ≤95. Laragh and Pickering were able to show that most of these patients were not hypertensive outside of the physician’s office, foreshadowing the description of “white coat” hypertension. They also discovered masked hypertension and nocturnal dipping. The three main advantages of performing an ABPM are:
- Ability to obtain multiple blood pressure readings
- Obtaining these readings outside of the clinic
- Obtaining readings from various times of the day and night
White Coat and Masked Hypertension

Figure 2. Classification of White coat and Masked hypertension
The white coat effect, when the blood pressure is high in the clinic but normal outside of the clinic, is well established. ABPM is required to truly make the diagnoses (though home blood pressure monitoring can be used as an alternative in some cases). White coat hypertension (see figure 2) is diagnosed when the office BP is above the threshold for diagnosis for hypertension, but the ABPM is not above this threshold (the exact numbers used traditionally are >140/90 for Office and >135/85 for ABPM). The importance of white coat is that it does not need to be treated with antihypertensive medications. Indeed, the SYST-EUR trial demonstrated that the benefits of treating hypertension were only seen in those with sustained hypertension, and not those with white coat hypertension. On the other hand, some of these individuals develop sustained hypertension over time. There was also a slightly higher risk of stroke observed in a longitudinal study of these patients, though it took six years for this trend to develop. Prudence suggests that these patients should not be discharged from the clinic but rather should receive continued follow up and monitoring.
Masked hypertension, when the blood pressure is okay in clinic but high out of the office, is somewhat more intriguing, less well understood, and even less commonly diagnosed. Given that masked hypertension falls into the Rumsfeldian “we don’t know what we don’t know” category, estimates of its incidence vary, and have been mentioned to be as high as 10% in the general population. In chronic kidney disease, Dr. Agarwal’s group reported the incidence of masked hypertension to be a whopping 33%! The presence of masked hypertension is associated with target organ damage (left ventricular hypertrophy and atherosclerotic plaques). Amongst patients with treated hypertension, those who are thought to be controlled on the basis of office BP, but truly have masked hypertension, have a greater than two-fold risk of future cardiovascular events. But who should be assessed for having masked hypertension? Anyone with target organ damage despite normal blood pressure or long term controlled hypertension raises an obvious red flag. Other individuals at high risk include those with diabetes, vascular disease, strong family of hypertension, and those with pre-hypertension. The high prevalence of masked hypertension in CKD suggest we should have a low threshold for doing ABPM.
Nocturnal Dipping
First described in 1988, nocturnal dipping refers to the drop in blood pressure seen at night in most individuals. Nocturnal dipping occurs due to decreased baroreflex threshold and decreased sympathetic nerve activity. The first report linked the lack of this drop with a greater risk of stroke; subsequent reports show an association of non-dipping status with left ventricular hypertrophy and cardiovascular mortality as well. Indeed, a sub-study from the HOPE trial showed that the timing of ramipril dosing and nocturnal blood pressure in the intervention arm could predict a substantial amount of the reduction in cardiovascular events seen. A group of Spanish investigators have reported successful conversion of non-dippers to dippers by changing the time when people take their blood pressure medication from morning to night. However, this has not been replicated by other researchers. Obstructive sleep apnea provides a unique therapeutic opportunity, where correction of sleep apnea reduces the sympathetic activity and blood pressure favorably.
Other Advantages of ABPM
There are other patterns seen on ABPM recordings which can help aid therapeutic decisions. Morning surge, often associated with extreme nocturnal dipping is associated with a high risk of stroke. Greater variability in blood pressure (similar to variability in heart rate or respiratory rate) is a good prognostic marker. One also gets a good idea of the heart rate, which can help in the titration of beta-blockers.
ABPM and clinical trials
Apart from diagnosing white coat and masked effect and providing an estimate of overall blood pressure load over 24 hours, the use of ambulatory blood pressure also provides multiple readings, thus eliminating regression to the mean that one might get with office BP measurement. For all these reasons, it has been the gold standard and has been used in clinical trials also. Apart from the aforementioned HOPE substudy, another great reminder of its utility was demonstrated with the renal denervation trials. The CONVERGE analysis demonstrated that traditionally, in placebo controlled trials, there is greater decrease in office blood pressure than in ambulatory blood pressure with intervention, implying information bias. In addition, regression to mean inflates the treatment effect in pre- and post-intervention comparisons (eg SYMPLICITY-HTN I), as nicely demonstrated in figure 3.
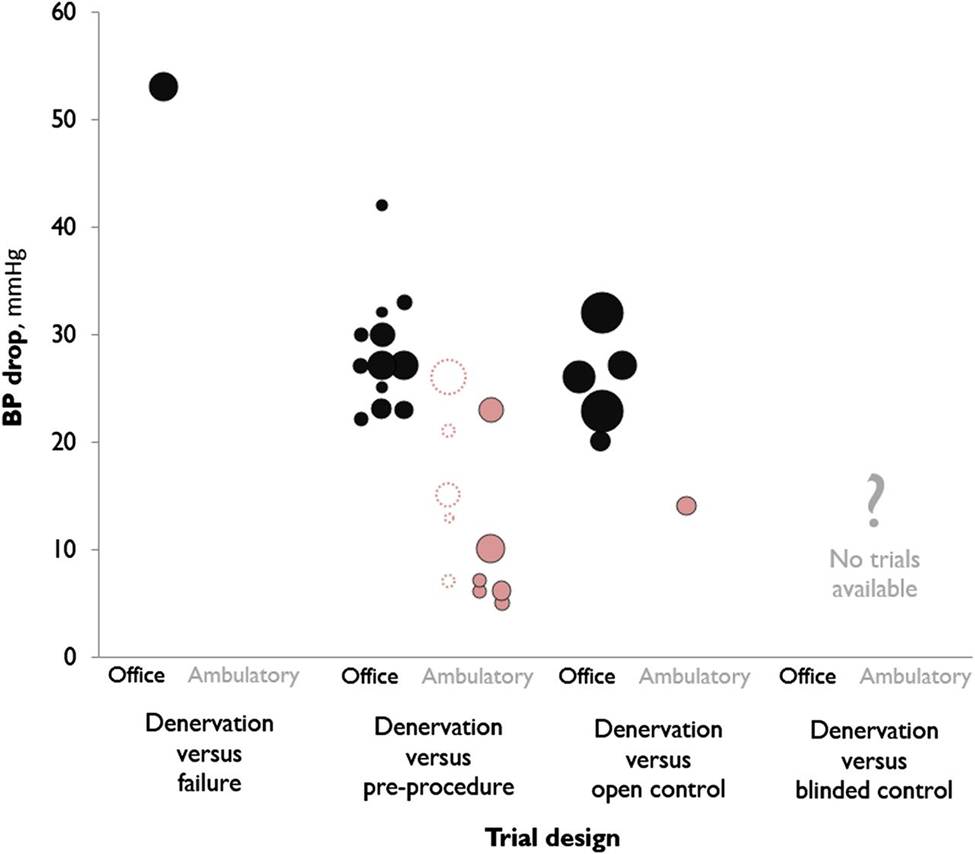
Figure 3: A plot showing the relationship between trial design and the reductions in office and ambulatory blood pressures. Each data point represents a trial. In unblinded trials, office pressure drops were 27.6 mm Hg versus pretreatment, and 26.6 mm Hg versus unintervened controls. Ambulatory pressure drops averaged 15.7 mm Hg across all trials. Dotted circles represent trials with atypical blood pressure measurement strategies and are discussed in the paper. This analysis was presented before SYMPLICITY HTN-3 (represented as ? in figure), and predicted that denervation would have little effect compared to blinded controls when ABPM was used. Reproduced from Howard et al, used with permission.
Disadvantages of ABPM
Cost and convenience are the two major disadvantages for routine ABPM. Though major guidelines recommend confirmation of the diagnosis of hypertension with out-of-office readings, the reimbursement for APBPM is not universal, despite a very good case based on cost-effectiveness modelling. The CMMS only covers it for diagnosis of white coat hypertension, whereas up north in Canada, it is not reimbursed despite rumors of universal healthcare.
Automated Oscillatory Blood Pressure (or the blood pressure measurement method used in SPRINT)
 Automated Oscillatory Blood Pressure (AOBP) is the one-and-done freshman who has come to challenge the seniors for a starting position on the Hypertension Assessment team. Could he bump ABPM, or even replace the gold standard of blood pressure measurement, the mercury sphygmomanometer. The father of AOBP is surely Martin Myers, from Sunnybrook Hospital in Toronto.
Automated Oscillatory Blood Pressure (AOBP) is the one-and-done freshman who has come to challenge the seniors for a starting position on the Hypertension Assessment team. Could he bump ABPM, or even replace the gold standard of blood pressure measurement, the mercury sphygmomanometer. The father of AOBP is surely Martin Myers, from Sunnybrook Hospital in Toronto.
There are a few simple principles underlying AOBP. The first is that the healthcare provider applies the cuff to the patient, switches it on to record the blood pressure and leaves the room so the patient is alone. The device can be programmed to start recordings after some (typically five minutes) time. This simulates a resting period in addition to the patient being alone to attenuate the white coat effect. In addition, the device takes multiple readings (typically 3 or 5), one every one to two minutes and displays the average. Two commonly used monitors are the BPTru Inc (Coquitlam, BC, Canada) and the Omron HEM 907 (Omron Corporation, Tokyo, Japan).
AOBP compared to Office Blood Pressure
In order to measure blood pressure properly, there are several key steps that should be followed:
- Patients should be seated in a chair with their backs supported and their arms bared and supported at heart level.
- Measurement should begin after at least 5 minutes of rest, palpation of the radial pulse, and use of an appropriate cuff size.
- Measurements should then be preferably taken with a mercury sphygmomanometer.
- Two or more readings separated by 2 minutes should be averaged. If the first two readings differ by more than 5 mmHg, additional readings should be obtained and averaged.
Does this really happen in the busy clinical reality? Not surprisingly, the answer is “No.” Blood pressure measured in most doctor’s’ offices is higher, by about 5 to 10 mm Hg, compared to a blood pressure measured in the same patient for a research study. In one of the largest trials of this nature, the CAMBO trial demonstrated that the AOBP measure was significantly more accurate than office blood pressure measures, and nearly eliminated the white coat effect. The table below shows the sequential blood pressures obtained in the study.

Figure 4. Sequential mean (SD) blood pressure readings taken every two minutes in 284 patients with BpTRU device during first routine office visit after enrolment into study. AOBP measured when patient is alone and resting are markedly lower than the first office BP. Average reading from 6 measurements is 10 mmHg lower for the systolic and 5 mmHg lower for the diastolic. Data from CAMBO trial.
AOBP compared to Ambulatory Blood Pressure
So, AOBP does give more accurate readings than the casual office measurement. But can it replace the ABPM? Surely it cannot provide us with data about nocturnal dipping, but how about the more common and vexing problems of white coat and masked hypertension? The CAMBO trial did suggest a marked attenuation in the incidence of both white coat and masked hypertension with the use of AOBP compared to office, which was supported by another group as well (see below). The exact thresholds used for diagnosis are an important consideration, and AOBP is not perfect, suggesting the two be used in conjunction rather than as alternatives.
| Systolic Target Achieved on ABPM (<135 mmHG mean daytime blood pressure) | ||||
| Yes | No | |||
| < 140 mmHG on BpTRU | Yes | 131 | 137 | Sens = 80%; Spec = 55% PPV = 49%; NPV = 84% |
| No | 32 | 170 | ||
| < 135 mmHG on BpTRU | Yes | 111 | 101 | Sens = 68%; Spec = 67% PPV = 52%; NPV = 80% |
| No | 52 | 206 | ||
| < 130 mmHG on BpTRU | Yes | 86 | 59 | Sens = 53%; Spec = 81% PPV = 59%; NPV = 76% |
| No | 77 | 248 | ||
| < 125 mmHG on BpTRU | Yes | 62 | 31 | Sens = 39%; Spec = 90% PPV = 67%; NPV = 73% |
| No | 101 | 276 | ||
| < 120 mmHG on BpTRU | Yes | 42 | 12 | Sens = 26%; Spec = 96% PPV = 78%; NPV = 71% |
| No | 121 | 295 | ||
Table 1. Two-By-Two Tables And BpTRU Predictive Characteristics For Achievement Of ABPM Systolic Target. Reproduced from Beckett and Godwin, used under CC by 2.0 license.
AOBP in Clinical trials and Guidelines
Though ambulatory blood pressure monitoring is considered the gold standard for BP measurement, the cumbersome, inconvenient, and expensive nature of doing those means that it is often performed only as an ancillary “sub-study”—or is being supplanted by home blood pressures, as was done in a recent PATHWAY-2 trial. AOBP presents an excellent opportunity, sort of the best of both worlds approach, by providing more accurate blood pressures than those usually performed in doctors’ offices, but still provided in a clinic setting. SPRINT was the first major trial which relied entirely on AOBP measures, and is likely not going be the last one to do so. The Canadian hypertension education programme guidelines already recommends using AOBP routinely in clinical practice.
Conclusion
AOBP represents a major advance in the measurement of blood pressure, and can potentially reduce white coat hypertension misdiagnosis, and may even allow us to pick up masked hypertension. Given the extra time taken, it would change clinic workflow if incorporated into routine practice. However, data suggests that its use in a waiting room (and not alone in a closed clinic room) also provides comparable results. With its validation by use in landmark trials and endorsement by hypertension guidelines, AOBP rollout seems imminent.
– Post written and edited by Dr. Swapnil Hiremath.




The problem of pseudo hypertension in the very elderly not discussed much how to approach?