NephMadness 2016: Recreational Drugs and the Kidney Region

Submit your picks! | For more on NephMadness 2016 | #NephMadness or #DrugsRegion on Twitter
“Eight hours work, eight hours sleep, and eight hours recreation”
– Brigham Young
“If Bread is the first necessity of life, recreation is a close second”
– Edward Bellamy
The teams in this region have indeed followed the above advice and incorporate the concept of leisurely, daily, recreational activity and evolved it into a successful exercise of pharmacologic science of Nobel Prize proportions. Do not overlook any of these four teams as they each have addictive potential to achieve a new high as they attempt to constrict, sclerose, necrose, and inflame their way to the title. Each competitor has demonstrated the talent and expertise to successfully elude the authorities and consistently stay one step ahead of federal marshals. Few fans may be aware of their nephrotoxic potential since none of their games are ever televised as they often take place behind closed doors and in the shadowy confines and recesses of backyards, gyms, clubs, homes, and workplaces. Barring any major arrests or overdoses, whichever team emerges from this recreational region will surely make a significant impact in corrupting the entire tournament.
Selection Committee member for the Recreational Drugs and the Kidney Region:
Mark A. Perazella, MD, FACP
Dr. Perazella is a Professor of Medicine in the Section of Nephrology at Yale University School of Medicine. He serves as Medical Director for the YNHH Acute Dialysis Unit and Medical Director of the Yale Physician Associate Program. He serves as Co-Director for the ASN Board Review Course and Update, is a member of the ASN Education and Post-Graduate Education Committees, and Chair for the ASN Onco-Nephrology Forum Group. He also serves on the Education Committee for the NKF. He is an Associate Editor for Clinical Journal of the American Society of Nephrology and Seminars in Dialysis, AKI Section Editor for Clinical Nephrology, and Core Curriculum Advisory Board member for the American Journal of Kidney Diseases. His clinical areas of interest include medication-induced kidney disease, cancer-related kidney disease, urine microscopy in kidney disease, AKI, and complications in ESRD such as nephrogenic systemic fibrosis and intradialytic hypotension.
Meet the Competitors for the Recreational Drugs and the Kidney Region
Synthetic Cannabinoids
Anabolic Steroids
Cocaine vs Ecstasy (MDMA)
Cocaine Nephrotoxicity
 This is without a doubt the #1 seed in this region, and let’s face it Cocaine’s fans make the Real Madrid soccer supporters look apathetic. With 17 million users worldwide (1.5 million in the US), and an additional 600,000 new fans each year, Team Cocaine can count on a strong home court advantage. First isolated from the Coca plant in 1860, Cocaine initially employed a solid but boring offense as a topical anesthetic literally numbing their opponents into submission. But Team Cocaine soon discovered its true calling, a triangle offense of serotonin, dopamine, and norepinephrine reuptake inhibition. The CNS and peripheral nicotinic acetylcholine receptors and serotonin receptors never have a chance to catch their breath as they undergo relentless upregulation. In 1961, the Single Convention of Narcotic Drugs, a worldwide treaty representing 185 countries, banned Team Cocaine from all recreational leagues as an illegal narcotic but this has not stopped them from engaging in private one-on-one competitions all around the world.
This is without a doubt the #1 seed in this region, and let’s face it Cocaine’s fans make the Real Madrid soccer supporters look apathetic. With 17 million users worldwide (1.5 million in the US), and an additional 600,000 new fans each year, Team Cocaine can count on a strong home court advantage. First isolated from the Coca plant in 1860, Cocaine initially employed a solid but boring offense as a topical anesthetic literally numbing their opponents into submission. But Team Cocaine soon discovered its true calling, a triangle offense of serotonin, dopamine, and norepinephrine reuptake inhibition. The CNS and peripheral nicotinic acetylcholine receptors and serotonin receptors never have a chance to catch their breath as they undergo relentless upregulation. In 1961, the Single Convention of Narcotic Drugs, a worldwide treaty representing 185 countries, banned Team Cocaine from all recreational leagues as an illegal narcotic but this has not stopped them from engaging in private one-on-one competitions all around the world.
Team Cocaine plays at a euphoric and highly stimulating pace never tiring from start to finish. Whether exposed through nasal insufflation, oral ingestion, intravenous infusion, or inhalation, Team Cocaine unleashes a devastating barrage of nephrotoxic injury. Leading the way as a cause of kidney injury is rhabdomyolysis with myoglobin associated ATN. Muscle ischemia as a result of direct vasoconstriction is the key element of surprise for the kidney as it never sees the myoglobin filtering due to its low molecular weight (16.7 kDa). Before the kidney can react, the proximal tubule is overwhelmed. In addition, Team Cocaine strangulates renal blood flow leading to segmental parenchymal infarction. Finally the systemic malignant hypertension induced by vasoconstriction can lead to endothelial injury, fibrinoid necrosis, a microangiopathic hemolytic anemia, and AKI. Team Cocaine is the vasoconstriction king and champion of ischemic nephrotoxicity!
Recently Team Cocaine drafted a cagey old veteran, levamisole, who was almost forgotten for the past 20 years but whose return has catapulted team Cocaine into an unstoppable force. The immunomodulatory and antihelminthic drug levamisole was permanently thrown out of the league in 1999 by the FDA due to severe agranulocytosis and aplastic anemia. In order to achieve cost control and higher profit margins, levamisole has now been introduced as a bulking agent for the majority of cocaine sold in the US. The combination of levamisole and cocaine has led to a new run and gun offense utilizing ANCA positive vasculitis as a mediator of nephrotoxicity. Levamisole leads to the development of both P-ANCA and C-ANCA as well as other autoimmune sequelae such as antiphospholipid antibodies and ANA. Focal necrotizing and crescentic glomerulonephritis with AKI has become a serious consequence when levamisole is in the game. Multiorgan vasculitic injury including pulmonary hemorrhage is the norm in levamisole-induced vasculitis. The pathognomonic calling card of levamisole vasculitis is a distinct violaceous retiform rash with a predilection for ischemia of the lower lobe of the ears. At best, the defense against levamisole-related ANCA vasculitis is restricted to nonspecific therapy using steroids, cytotoxic therapy, and possible B-cell depleting agents.
Team Cocaine with or without levamisole in the lineup is a formidable opponent against the kidney with few weaknesses beyond the use of federal regulation and societal pressures to prevent the team from ever taking the court. Otherwise, once the game starts…the nephrons don’t stand a chance!
Ecstasy
 It’s hard not to like a socially empathetic team like Ecstasy that extols the sensation of bliss and tranquility and the dream of Shangri-La. However, imagery can be deceiving and Team Ecstasy does not hallucinate when it comes to causing severe electrolyte disorders, most impressively hyponatremia and to a lesser degree AKI. While other teams attempt to directly injure the glomerulus or tubules, Team Ecstasy takes a different approach and focuses on breaking the kidney’s ability to regulate water balance. With a worldwide following of 0.2% to 0.6% of the global population, especially popular among young adults, Team Ecstasy enjoys rave reviews particularly at electronic dance establishments.
It’s hard not to like a socially empathetic team like Ecstasy that extols the sensation of bliss and tranquility and the dream of Shangri-La. However, imagery can be deceiving and Team Ecstasy does not hallucinate when it comes to causing severe electrolyte disorders, most impressively hyponatremia and to a lesser degree AKI. While other teams attempt to directly injure the glomerulus or tubules, Team Ecstasy takes a different approach and focuses on breaking the kidney’s ability to regulate water balance. With a worldwide following of 0.2% to 0.6% of the global population, especially popular among young adults, Team Ecstasy enjoys rave reviews particularly at electronic dance establishments.
Also known as 3,4-methylenedioxy-methamphetamine (MDMA) or Molly, Team Ecstasy’s offensive strategy is the double team. With simultaneous reuptake inhibition and enhanced neurotransmitter release, serotonin, dopamine, and norepinephrine deluge the CNS leading to the desired euphoric and entactogenic state at the expense of hyperstimulation of the autonomic nervous system. Team Ecstasy may be the hottest competitor in the field leading to intense thermogenesis that increases thirst and water intake. Some Ecstasy users prophylactically ingest large volumes of free water anticipating increased sweating and hyperthermia after dosing. This is precisely the move and countermove team Ecstasy wants and the intricate trap has been set. Now MDMA directly stimulates ADH secretion lowering free water clearance of the kidney and soon after the sodium concentration crashes. This leads to cerebral edema, seizures, and brain stem herniation.
Team Ecstasy is particularly effective in young premenopausal women where estrogen decreases cellular Na-K ATP pump activity and so they are less able to protect themselves from osmotic fluid shifts in hyponatremia. Additionally young women have exaggerated vasoconstrictive response to ADH leading to decreased cerebral blood flow. An additional group that may inherently be more sensitive to the complications of ecstasy are those individuals with a genetic polymorphism of the cytochrome P450 isoenzyme CYP2D6, which is responsible for elimination of MDMA.
To add further acute kidney injury to hyponatremic insult, Team Ecstasy can cause nontraumatic rhabdomyolysis through the development of hyperthermia coupled with intense physical exertion (nonstop dancing at electronic music clubs/concerts), vasoconstriction, and volume depletion. This results in myoglobin induced ATN.
Team Ecstasy has also been known to attempt multiple illegal substitutions during the game. Although they may wear the same jersey and go by the name “Ecstasy,” some teams do not contain MDMA at all but rather multiple novel psychoactive products such as aminoindanes, piperazines, and pipradrol derivatives. No specific electrolyte or kidney abnormalities have yet been reported with these alternative compounds.
However you look at it Team Ecstasy brings to the court a multidimensional array of kidney and electrolyte abnormalities that cannot be underestimated. At present there is no specific defense that can be mounted to prevent these nephrologic complications other than forfeiting the game and not showing up to party! Bottom line….play and dance at your own risk!
Synthetic Cannabinoids vs Anabolic Steroids
Synthetic Cannabinoids (SCB)
 Team SCB is the designer competitor in the tournament with an ever changing starting lineup taking full advantage of scientifically enhanced player characteristics. This team was synthesized to win! Not satisfied with traveling to Colorado to get legal cannabis and enjoy the benefits of its active metabolite tetrahydrocannabinol (THC) on the Cannabis receptors 1 and 2 (CB1R and CB2R), Team SCB was formed in 2004. The goal of Team SCB was to create synthetic compounds that more efficiently compete for the same CB receptors without the need for THC. For the past decade, Team SCB has enjoyed international attention for its ability to induce intense euphoria, delirium, psychosis, and hallucinations unrivaled even when compared to standard THC. Most importantly, team SCB remained under the radar because the standard toxicology test for THC could not detect these novel molecules.
Team SCB is the designer competitor in the tournament with an ever changing starting lineup taking full advantage of scientifically enhanced player characteristics. This team was synthesized to win! Not satisfied with traveling to Colorado to get legal cannabis and enjoy the benefits of its active metabolite tetrahydrocannabinol (THC) on the Cannabis receptors 1 and 2 (CB1R and CB2R), Team SCB was formed in 2004. The goal of Team SCB was to create synthetic compounds that more efficiently compete for the same CB receptors without the need for THC. For the past decade, Team SCB has enjoyed international attention for its ability to induce intense euphoria, delirium, psychosis, and hallucinations unrivaled even when compared to standard THC. Most importantly, team SCB remained under the radar because the standard toxicology test for THC could not detect these novel molecules.
Team SCB has a truly imposing roster consisting of Spice, K2, Bliss, Black Mamba, Bombay Blue, Genie, and Zohai. Each of these organic players is structurally unique, yet share the prolonged agonist capacity for the CB1 and CB2 receptors. In fact the farm system for bringing up new players is extensive and currently there are over 50 identified rookie molecules already playing in the minor leagues and ready to move up to the big leagues. New SCB players are being created at a feverish pace across the world and have been labeled as NPS (new psychoactive substances) each with its own unique chemical structure to avoid legal oversight and forensic detection.
Team SCB has often been referred to as herbal incense, bath salts, or plant feeders and were initially available at gas stations, incense shops and convenience stores where they were sold mixed with natural herbs to be smoked or inhaled. Currently, internet sales of these products is a major route of distribution. In spite of the clear label on the packages stating not for human consumption, SCB became widely popular particularly among male high school students and are now marketed for use with e-cigarettes.
Initially team SCB was relegated strictly to the Psychotropic and Addiction League, however it soon became clear that they were too good for that competition and they really deserved to be promoted into the Nephrotoxic League. What happened? How do you go from a simple cannabis look-alike to competing in the big show with major league Nephrotoxins? Let us investigate…
CBR have now been found not just in the CNS but also in the renal podocytes, endothelial cells, mesangial cells, and proximal tubules. Endogenous endocannabinoids may play an important role in normal renal physiology and on the pathogenesis of diseases such as diabetic nephropathy. Through mechanisms that have not yet been defined, differential stimulation of CB1R and CB2R by SCB, in contrast to THC and endogenous cannabinoids, leads to direct tubular injury and ATN. This nephrotoxic effect appears to be independent from hypotension, rhabdomyolysis, or the presence of adulterated compounds such as NSAIDs. Kidney biopsies from a select cohort of SCB users with AKI showed acute interstitial nephritis in 10% with the majority of patients showing ATN. In this series, 20% of patients required temporary hemodialysis.
Defensive measures to protect the kidney from team SCB are underway in the form of CBR antagonists but this strategy is not yet ready for prime time. Right now, team SCB is limited only by the individual legal restrictions that vary by country but include Schedule 1 designation of the Controlled Substances Act in the US to bans on individual compounds such as Spice or a complete ban of all homologues of THC.
It is clear that team SCB must be given credit for being diverse and inventive with an ever changing game strategy and an as yet unknown and unstoppable mechanism for causing renal injury. This team definitely spices up the tournament.
Anabolic Steroids
 The most powerful team flexing their muscles in the tournament is Team Anabolic Steroids with their motto “we are here to pump you up” and their Olivia Newton John theme song “Let’s Get Physical.” Clearly intimidating their opponents with androgenic arrogance, Team Anabolic Steroids is all the rage worldwide and enjoys the support of up to 3% of young males (3-4 million in the US), almost half of all competitive weightlifters, and many track and field and professional athletes. Famous Team Anabolic Steroid supporters include Arnold Schwarzenegger, Lance Armstrong, Barry Bonds, Mark McGuire, Hulk Hogan, Ben Johnson, and scores of Olympic Eastern European weightlifting teams from the 70s and 80s.
The most powerful team flexing their muscles in the tournament is Team Anabolic Steroids with their motto “we are here to pump you up” and their Olivia Newton John theme song “Let’s Get Physical.” Clearly intimidating their opponents with androgenic arrogance, Team Anabolic Steroids is all the rage worldwide and enjoys the support of up to 3% of young males (3-4 million in the US), almost half of all competitive weightlifters, and many track and field and professional athletes. Famous Team Anabolic Steroid supporters include Arnold Schwarzenegger, Lance Armstrong, Barry Bonds, Mark McGuire, Hulk Hogan, Ben Johnson, and scores of Olympic Eastern European weightlifting teams from the 70s and 80s.
Team Anabolic Steroids uses a simple straightforward strategy to achieve anabolic (muscle building) and androgenic (masculinizing) properties consisting of a high protein intake (> 3 g/kg/day) coupled with a variety of supraphysiologic doses of natural and synthetic testosterone derivatives. Polypharmacy is often the normal playbook and it is not unusual for Team Anabolic Steroid players to work together in a tag team match with Team Cocaine and even throw in a little growth hormone and NSAIDs to seal the victory. Most players on team Anabolic Steroids are known as APED (Appearance and Performance Enhancing Drugs) and can be recruited as free agents easily off the internet.
No organ is spared the potential toxicity of APEDs, including neuropsychiatric disease, suppression of the hypothalamic-pituitary-testicular (HPT) axis, left ventricular hypertrophy, and cardiomyopathy, hepatic steatosis, hypertension, atherosclerosis, hypercoagulability, malignancy, and, of course, nephrotoxicity. Team Anabolic Steroids has only recently entered the Nephrotoxic League and their lesion of choice: FSGS.
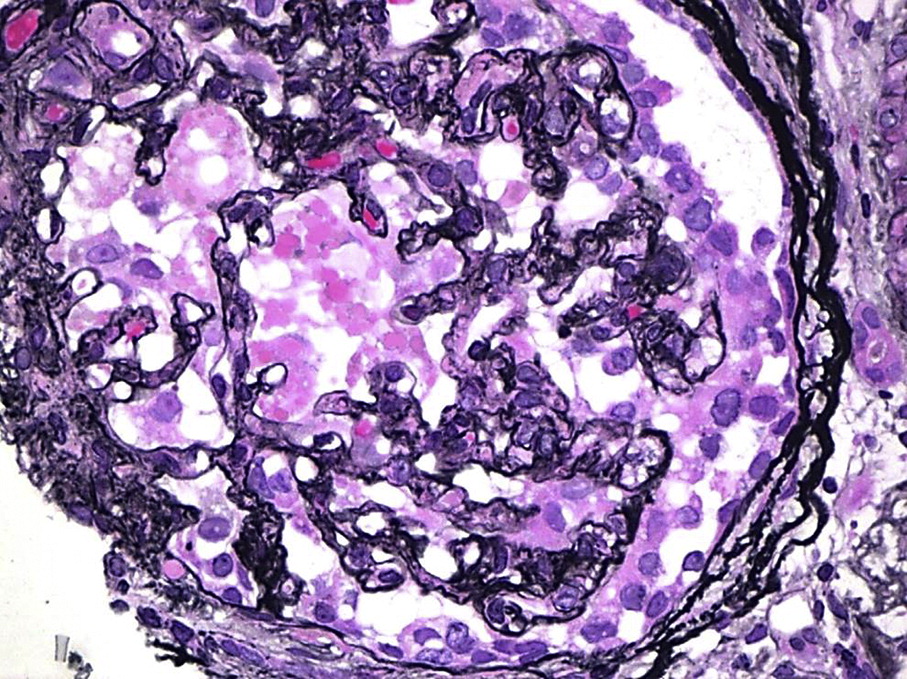
For more on Collapsing GN, visit AJKD’s Atlas of Renal Pathology II
Initially it was thought that FSGS lesions seen with APEDs resulted from increased metabolic and hyperfiltration strain put on glomeruli and podocytes from the high protein intake and massive physical size of the players. However, the degree of podocyte injury and effacement as well as the presence of collapsing FSGS in 30% of biopsies instead of the typical perihilar and tip lesions seen with hyperfiltration suggest a direct effect of anabolic steroids on the podocyte. In fact testosterone excess experimentally can induce podocyte apoptosis, subsequent glomerulosclerosis, and albuminuria.
Although the best defense against FSGS has been developed and implemented by KDIGO, there is no experience on the success of this strategy on the unique brand of FSGS that team Anabolic Steroids employs.
In a recent game, Team Anabolic Steroids introduced a new offensive strategy of AKI. Four opposing team players developed stage 2 AKI according to the AKIN classification and recovered after discontinuing all steroid injections. No interstitial nephritis was noted so a direct tubulotoxic effect has been postulated for anabolic steroids. This is the second time a series of AKI has been reported from anabolic steroids. In addition, AKI from anabolic steroids could occur secondarily as a consequence of multiorgan failure or steroid-induced liver disease. The AKI option of nephrotoxicity for team Anabolic Steroids coupled with the risk of FSGS clearly makes it a worrisome opponent to face.
Team Anabolic Steroids has been under constant scrutiny by the World Anti-Doping Agency (WADA) and has evolved a mechanism to avoid detection through genetic polymorphisms. The current key to detection of anabolic steroids is by measuring the urine ratio of testosterone and epitestosterone (T/E ratio test) and any ratio > 4 indicates exogenous androgen supplementation and is valid enough to warrant disqualification and short- or long-term bans from competition. Team Anabolic Steroids has developed a genetic polymorphism using a deletion of the UGT2B17 liver enzyme responsible in producing the phase I glucuronidation of testosterone so it is excreted in the urine. Players with this polymorphism (primarily white and Asian) never exceed a T/E ratio of 4:1 as testosterone is not freely filtered by the kidney allowing them to go under the radar. A truly deceptive and innovative approach which keep them in the game and enhance their potential for nephrotoxicity!
Team Anabolic Steroids will not get pushed aside easily by any other competitor. Time to get ready to rumble!
– Post written and edited by Dr. Warren Kupin.


This review is really awesome! I never knew that Synthetic Cannabinoids are implicated in kidney injury. Thanks for the article