My Blood Pressure on Dialysis is 150/80. I Feel Great but My Nephrologist Doesn’t!
Blood pressure control in chronic kidney disease (CKD) and end stage renal disease (ESRD) patients has been a challenge for most nephrologists. Hypertension is a well-known risk factor for cardiovascular disease and death in the general population, whereas paradoxically, low blood pressure (BP) has been associated with higher mortality in dialysis patients. Many have described a reverse J-shaped curve for association of systolic blood pressure (SBP) and mortality per-dialysis. In a recent AJKD article, Sumida et al illustrate in their observational study the effect of blood pressure before initiation of dialysis and the effect on mortality.
Sumida et al did an observational study of over 17,000 US veterans initiating dialysis. In this large national cohort, they found a reverse J-shaped association of SBP over the 1-year pre-dialysis period with all-cause mortality following dialysis therapy initiation, independent of most other predictors. Most strikingly, they found that the patients with predialysis SBPs < 140 mm Hg had significantly higher death risks after dialysis therapy initiation. These associations were most robust for mortality within the immediate 3 months following the dialysis transition. In contrast, predialysis diastolic blood pressure (DBP) showed no consistent association with post-dialysis mortality. In the pre-analysis selected subgroups, the authors found statistically significant interactions were present for body mass index (BMI), congestive heart failure (CHF), and estimated glomerular filtration rate (eGFR), with greater contributions of lower SBP to mortality among patients with BMI > 30 kg/m2, those with CHF, and those with a last eGFR > 10 mL/min/1.73 m2.
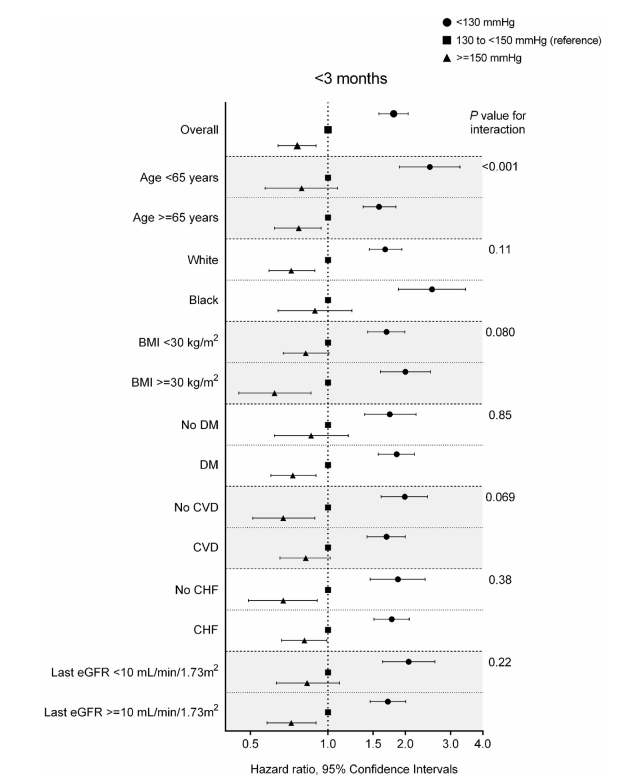
Adjusted hazard ratios (95% confidence intervals) of all-cause mortality in the first 3 months after dialysis therapy initiation associated with predialysis systolic blood pressure categories in selected subgroups. Model is adjusted for age, sex, race/ethnicity, marital status, comorbid conditions (cardiovascular disease [CVD], congestive heart failure [CHF], peripheral vascular disease, lung disease, diabetes mellitus [DM], liver disease, and Charlson Comorbidity Index score), body mass index (BMI) averaged over the 1-year predialysis period, estimated glomerular filtration rate (eGFR) slope, last eGFR before dialysis therapy initiation, medications (angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, β-blockers, calcium channel blockers, vasodilators, diuretics, statins, and erythropoiesis-stimulating agents), cardiovascular medication adherence, and type of vascular access (arteriovenous fistula, arteriovenous graft, or catheter). Figure 2 from Sumida et al, AJKD © National Kidney Foundation.
- This is an observation study and does not establish causality. Underlying cardiac disease could be the major link between reduced blood pressure and mortality.
- The patients were mostly male veterans.
- Introduction of medications related to non-nephrology providers were not accounted for.
While the first two limitations are self-evident, the third limitation is very important in clinical practice. This study highlights that “transitions” of care is a very important component that nephrologists need to pay strict attention to. When CKD patients transition to ESRD, there are many variables that make the patient vulnerable to a very turbulent start on dialysis. Examples can be related to “access complications”, “cardiac arrhythmias“, and most importantly, “CHF”. Blood pressures often drop after starting dialysis due to improved volume control, with many patients able to discontinue their antihypertensives after initiating renal replacement therapy. Medications can be introduced sporadically by many different physicians for good reasons in the predialysis period leading to effect on BP control.
In addition, many times, the electronic medical records (EMR) are not necessary communicative and illustrative of those changes. Dialysis initiation should lead to a “mandatory” medication reconciliation done in the first 3 months. Most dialysis EMRs are not in sync with the “clinic” EMRs and medications might be introduced by cardiologists and internists without the knowledge of the nephrologist and could lead to overzealous correction of the BP. Discontinuation of certain BP medications might be critical in the early ESRD time frame as ultrafiltration becomes a method for BP control. Such small but important practices can perhaps impact patient mortality.
I applaud the authors on showcasing this important finding. Future clinical trials are needed to clarify the ideal predialysis SBP and determine what can be done to decrease this early mortality seen among incident dialysis patients.
– Post prepared by Kenar Jhaveri, AJKD Social Media Advisory Board member. Follow him @kdjhaveri.
To view the Sumida et al article abstract or full-text (subscription required), please visit AJKD.org.
Title: Blood Pressure Before Initiation of Maintenance Dialysis and Subsequent Mortality
Authors: K. Sumida, M.Z. Molnar, P.K. Potukuchi, F.Thomas, J.L. Lu, MD, V.A. Ravel, M. Soohoo, C.M. Rhee, E. Streja, J.J. Sim, K. Yamagata, K. Kalantar-Zadeh, C.P. Kovesdy
DOI: 10.1053/j.ajkd.2016.12.020


This title is misleading and being retweeted misleadingly. The predictor here is average BP within 1 year prior to dialysis initiation, not the BP at the start of treatment. The title suggests that 150/80 is the BP being taken during or at start of dialysis.