Pruning Polypharmacy: Pill Pushers to Deprescribers in Dialysis?
The Causes and Consequences of Polypharmacy
When faced with a patient who has a symptom, or a clinical or even laboratory abnormality, the natural tendency for a physician is to prescribe something, anything, in a genuine effort to alleviate the problem. Indeed, we even use the placebo effect knowingly: this survey of about 800 primary care providers (PCPs) from the United Kingdom reports that 12% of PCPs use ‘pure’ placebos (sugar pills etc) and almost all PCPs (97%) admitted to using ‘impure’ placebos (vitamins, antibiotics for viral infections, and such).
In chronic diseases, this tendency to manage each symptom with a pill (often, multiple pills), as well as management of adverse effects with more pills, very quickly results in polypharmacy. Apart from the fact that some of these pills might not just be placebos, and ineffective placebos at that, polypharmacy can easily result in clinically important drug interactions, especially in patients with decreased renal clearance. The burden of more pills is acutely faced by our patients, and pill burden directly associates with decreased quality of life in patients, even more so than the symptoms of chronic kidney disease.

Photo: Pixabay / qimono
Pill Burden in Dialysis: the Extent of the Problem and a Potential Solution
How big is the problem of polypharmacy? Imagine swallowing 19 pills daily, which was the amount reported as the median intake in this study from 2009 in maintenance dialysis patients. A quarter of the patients were actually prescribed to take more than 25 pills per day. They can hardly be blamed for not taking all of them – adherence (assessed by pharmacy refills) was less than 40%. This brings up the potential cure for the disease of polypharmacy – if patients are non-adherent, why not take the obvious step and actively stop medications?
The ‘deprescribing’ movement has really taken off in the last few years since the first use of the term in 2003. Deprescribing is defined as “the process of withdrawal of an inappropriate medication, supervised by a health care professional with the goal of managing polypharmacy and improving outcomes” in a 2015 systematic review. Though initially described and implemented in the geriatric population where the dangers of polypharmacy are well-recognized, deprescribing is a logical strategy in patients with chronic diseases such as the dialysis population. This intervention was evaluated in a quality assurance study by McIntyre et al, recently published in AJKD.
Deprescribing in Dialysis
McIntyre et al developed a deprescribing tool and implemented it in 240 hemodialysis patients while monitoring patient safety and satisfaction. The 5 medications chosen for deprescribing were: diuretics, statins, quinine, alpha-1 blockers, and proton pump inhibitors (PPI). The first two were deprescribed based on lack of efficacy, and the last three for safety concerns. (See the supplementary information for detailed explanations of the rationale behind choosing these 5 medication classes).
Interestingly, although phosphate binders contribute to roughly half of the pill burden in a previously reported study, they were not chosen for deprescribing, likely related to their perceived benefits. Secondly, of the 171 patients taking one of these medications, the majority (100) had a good clinical reason to take the pill; hence, no attempt was made to deprescribe. In the remaining 71 patients, deprescribing could not be done in about half of them; in some cases, the patients were not willing (PPI and reflux symptoms), whereas in 16 patients, an assessment of urine volume could not be done to stop diuretics. (As an aside, residual function is a very robust predictor of clinical outcomes in dialysis, though the benefit of diuretics to keep it going has not been shown that conclusively).
How successful was the deprescribing? Overall, 31 medications out of the 40 flagged in the algorithm were stopped in 27 patients, making for a success rate of 78%. Though statins were used commonly (95 patients were on a statin), this was appropriate in all but one patient. The few patients on alpha blockers and quinine underwent successful deprescribing, and 75% of the PPI users also were able to discontinue the medication.
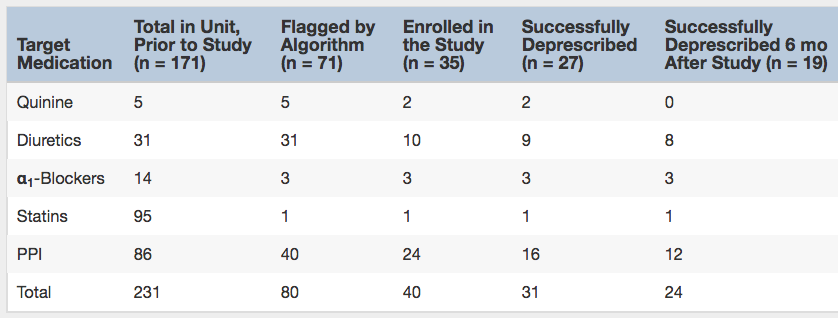
Number of Patients Taking a Target Medication Throughout the Deprescribing Study. Note: Patients may be taking more than one target medication (eg, diuretic with a PPI). One patient who had discontinued 2 medications (quinine and PPI) died 5 months after the study and could not be included in the 6-month follow-up. Table 3 from McIntyre et al, AJKD © National Kidney Foundation.
Take-Home Messages
This study by McIntyre et al shows that it is possible to safely deprescribe medications in dialysis patients using a carefully crafted algorithm. Most of the work undertaken here seems to be done by pharmacists, which highlights the critical role they could play if widely utilized. Another key aspect is not to bluntly stop a medication, but to critically question its appropriateness in an individual. This can also be a weakness, especially for PPIs, as the authors point out that it is challenging to determine the real indication behind prescribing a medication in the first place in order to safely deprescribe it.
Nevertheless, this study demonstrates that a relatively simple process can reduce some of the polypharmacy burden of our patients. Indeed, the 2003 paper that first used the term deprescribing had a very sensible description of the process: 1) review all current medications, 2) identify medications to be ceased, substituted, or reduced, 3) plan a deprescribing regimen in partnership with the patient, and 4) frequently review and support the patient. Amen.
– Post prepared by Swapnil Hiremath, AJKDBlog Contributor. Follow him @hswapnil.
To view the McIntyre et al article abstract or full-text (subscription required), please visit AJKD.org.
Title: Targeted Deprescribing in an Outpatient Hemodialysis Unit: A Quality Improvement Study to Decrease Polypharmacy
Authors: C. McIntyre, R. McQuillan, C. Bell, and M. Battistella
DOI: 10.1053/j.ajkd.2017.02.374

Nice post.