Reaching Renal Replacement Therapy Targets Through Quality Improvement Initiatives: A Success Story
Acute kidney injury (AKI) is common in hospitalized patients and is associated with high morbidity and mortality, especially if requiring renal replacement therapy. Continuous renal replacement therapy (CRRT) is indicated in patients who are hemodynamically unstable and it is the responsibility of the nephrologist to ensure proper dosing. Clinical practice guidelines for CRRT dosing are provided by KDIGO and KDOQI and are based on urea clearance, which is a function of the effluent flow rate. KDIGO and KDOQI recommend an effluent flow rate of 20-25 mL/kg/hour, with a level 1A recommendation. The ATN and RENAL studies (published in NEJM in 2008 and 2009, respectively) demonstrated that in patients with critical illness and AKI, higher intensity CRRT (at 30-40 mL/kg/hr) did not improve mortality, renal recovery, or rates of non-renal organ failure compared to CRRT at 20 mL/kg/hr. It is also important to consider adverse effects of overdosing CRRT, including effects on medication clearance, electrolyte balance, and utilization of resources.
A 2002 study by Venkataraman, et al found that in one large, tertiary care hospital, the average delivered dose of CRRT was significantly lower than what was prescribed (68% of the prescribed dose actually delivered). In 2013, Koyner, et al surveyed practicing nephrologists in the United States and found that only 15% of patients with AKI requiring hemodialysis had assessment of dialysis dose (such as Kt/V). Assessment of CRRT dosing was not addressed in the survey but it was noted as an important area for future study.
Although we can calculate the weight-based dose needed to achieve 20-25 mL/kg/hr, researchers at the University of Colorado Hospital (UCH) discovered that many patients were not in fact achieving the target dose. UCH is a large academic medical center which performs 1,200-1,500 CRRT treatments each year, prescribed by a nephrology fellow and attending and performed by an intensive care unit (ICU) nurse. In a recent study published in AJKD, Griffin et al share the results of a quality improvement (QI) study to assess the impact of various modifications on the percentage of CRRT treatments meeting the target dose.
The study began with retrospective chart review to determine the weekly percentage of CRRT treatments with an average dose of 20-25 mL/kg/hr. A multidisciplinary task force then identified barriers to achieving adequate dosing, such as accuracy of data collection and entry into the EMR, barriers in communication between physicians and nurses, and lack of dosing information in the EMR order set and procedure note template.
Next, interventions were designed to overcome these barriers, including automating EMR calculations, training nurses to standardize data input, creating a protocol for nephrology fellows and attendings, and modifying the EMR order set and note template. As an example of standardizing data input, nurses were advised to document an effluent rate of zero to indicate time off of CRRT (such as when the filter clotted or during physical therapy or when off the floor for studies).
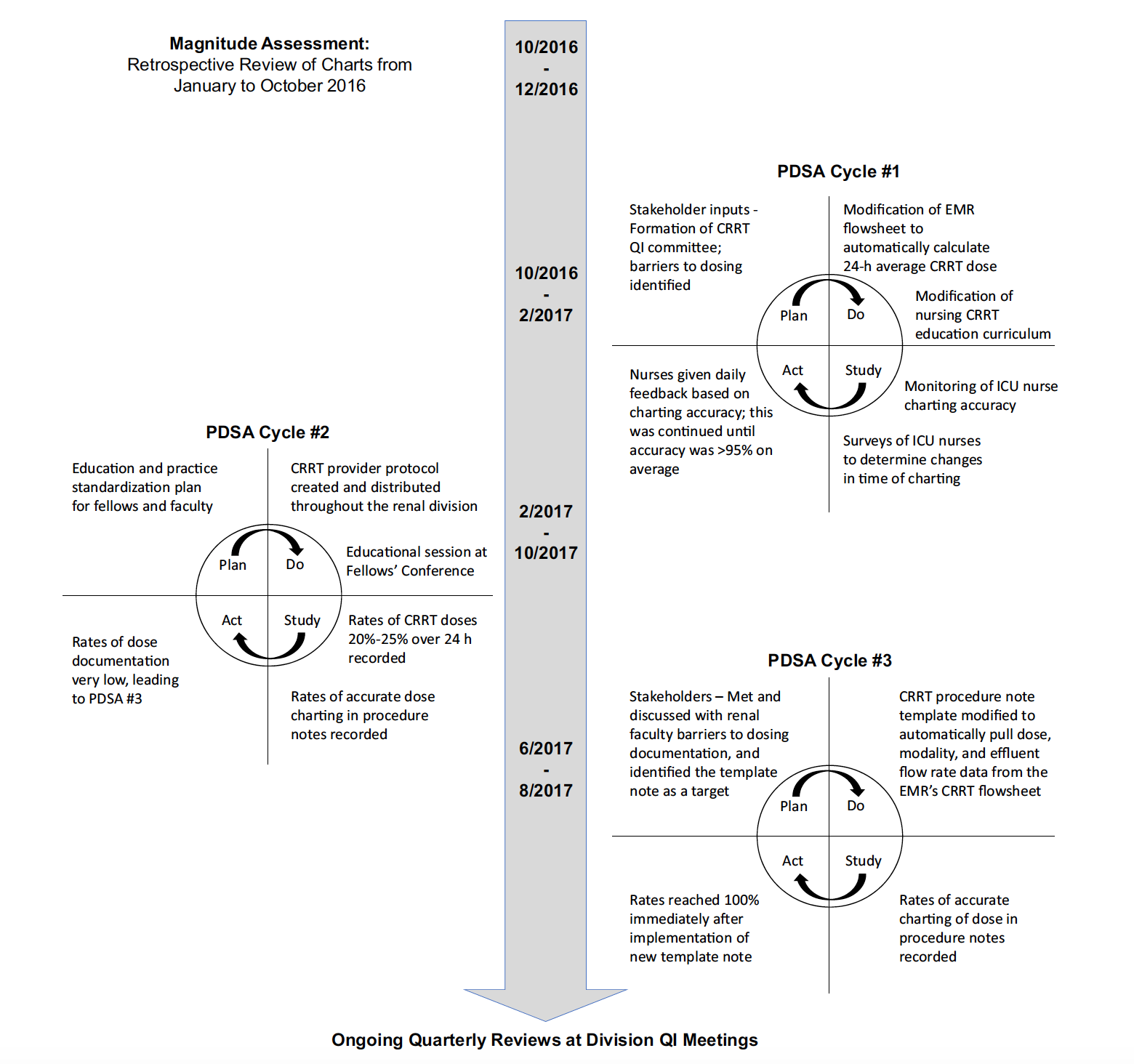
Timeline of major quality improvement (QI) interventions. Abbreviations: CRRT, continuous renal replacement therapy;
EMR, electronic medical record; ICU, intensive care unit; PDSA, Plan-Do-Study-Act. Figure 2 from Griffin et al, AJKD © National Kidney Foundation.
The primary outcome was the percentage of treatments per week achieving the target dose. Secondary measures were mortality, length of ICU and hospital stay, and number of CRRT treatments. The QI team monitored process measure such as accuracy of data entry and percentage of nephrology attending notes which addressed the average CRRT dose from the previous day (automatically pulled into the note), including, importantly, whether the dose needs to be adjusted. Nurses were also surveyed at random to assess for an undesirable increase in nurse charting time.

Control chart before and after intervention implementation. Figure 3 from Griffin et al, AJKD © National Kidney Foundation.
The interventions had a big impact. Before implementation of these interventions, 9% of treatments were excluded from the study entirely as dosing could not be calculated with the available data. Pre-intervention, only 33% of treatments were in the desired dose range and notably, 22% were dosed much higher than recommended, above 30 mL/kg/hr. After the implementations, the percentage of treatments achieving the goal dose doubled to 66%, with a corresponding significant decrease in underdosed and highly overdosed treatments (down to 12% and 4%, respectively).
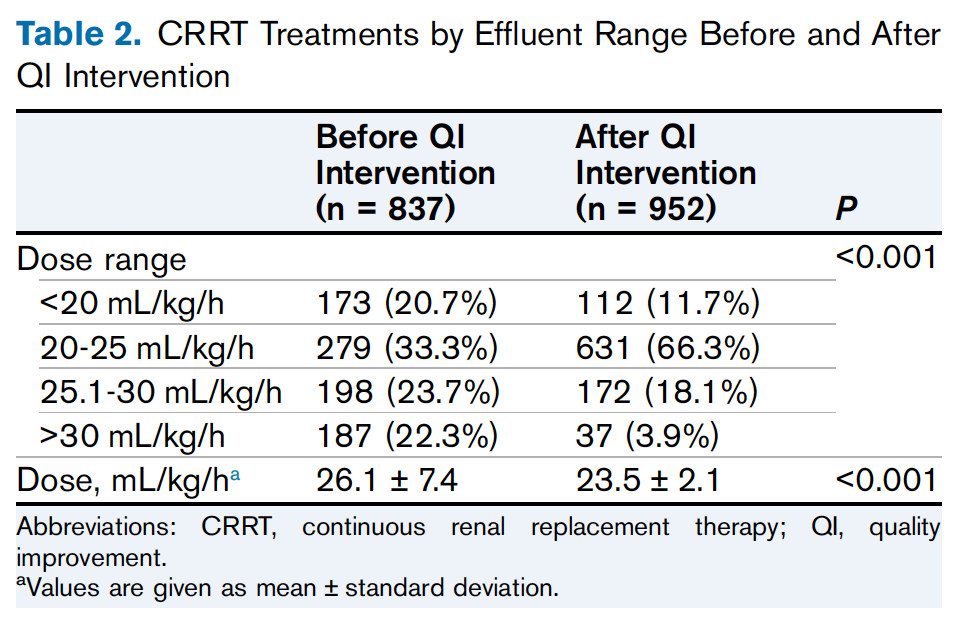
Table 2 from Griffin et al, AJKD © National Kidney Foundation.
The only secondary outcome that changed was mortality, down from 60% to 45%. Data accuracy and dosing documentation by attendings improved and nurses did not report an increase in their workload.

An example of the CRRT dosing flowsheet following the quality improvement intervention. Abbreviation: CVVH, continuous venovenous hemofiltration. Figure 1 from Griffin et al, AJKD © National Kidney Foundation.
This QI initiative doubled the rate of compliance with practice guidelines for CRRT dosing. Both underdosing and overdosing were reduced, with important implications for antimicrobial clearance, electrolyte balance, and other outcomes affecting morbidity and mortality. Griffin et al reflected on whether it is possible to move toward 100% compliance with CRRT dosing, noting that critical care is dynamic and can be unpredictable, making it inherently difficult to predict CRRT downtime. Thus, interventions to prolong circuit life and prevent clotting may be another area for improvement.
The purpose of national guidelines is to standardize evidence-based practices, in part by guiding physicians to prescribe effective treatments at optimal dosages. This study demonstrated the many ways patients may not receive the treatments we prescribe as intended, which has important implications for morbidity and mortality. As nephrologists, though we practice in a variety of clinical settings, we share the goal of achieving the best outcomes for our patients. System-wide evaluation and modification are crucial; in an accompanying editorial in AJKD, Neyra and Tolwani describe specific factors that will make further CRRT-focused QI initiatives successful. However, each of us also have the personal ability and responsibility to participate in quality improvement in our daily practice, starting as simply as assessing and improving the way we communicate.
– Post prepared by Diana Mahbod, AJKDBlog Contributor. Follow her @DiMiRenalMD.
To view Griffin et al (subscription required), please visit AJKD.org.
Title: Continuous Renal Replacement Therapy Dosing in Critically Ill Patients: A Quality Improvement Initiative
Authors: B.R. Griffin, A. Thomson, M. Yoder, I. Francis, S. Ambruso, A. Bregman, M. Feller, S. Johnson-Bortolotto, C. King, D. Bonnes, L. Dufficy, C. Wu, A. Bansal, D. Tad-y, S. Faubel, and D. Jalal
DOI: 10.1053/j.ajkd.2019.06.013

Leave a Reply