Highlights from the February 2023 Issue
Editor’s Note: We asked authors of Original Investigations to provide short plain-language summaries that would briefly summarize what inspired their study, the basic approach taken, what was learned, and why it matters. We hope our readers will find this valuable in helping them keep up with the latest research in the field of nephrology. From the February 2023 issue:
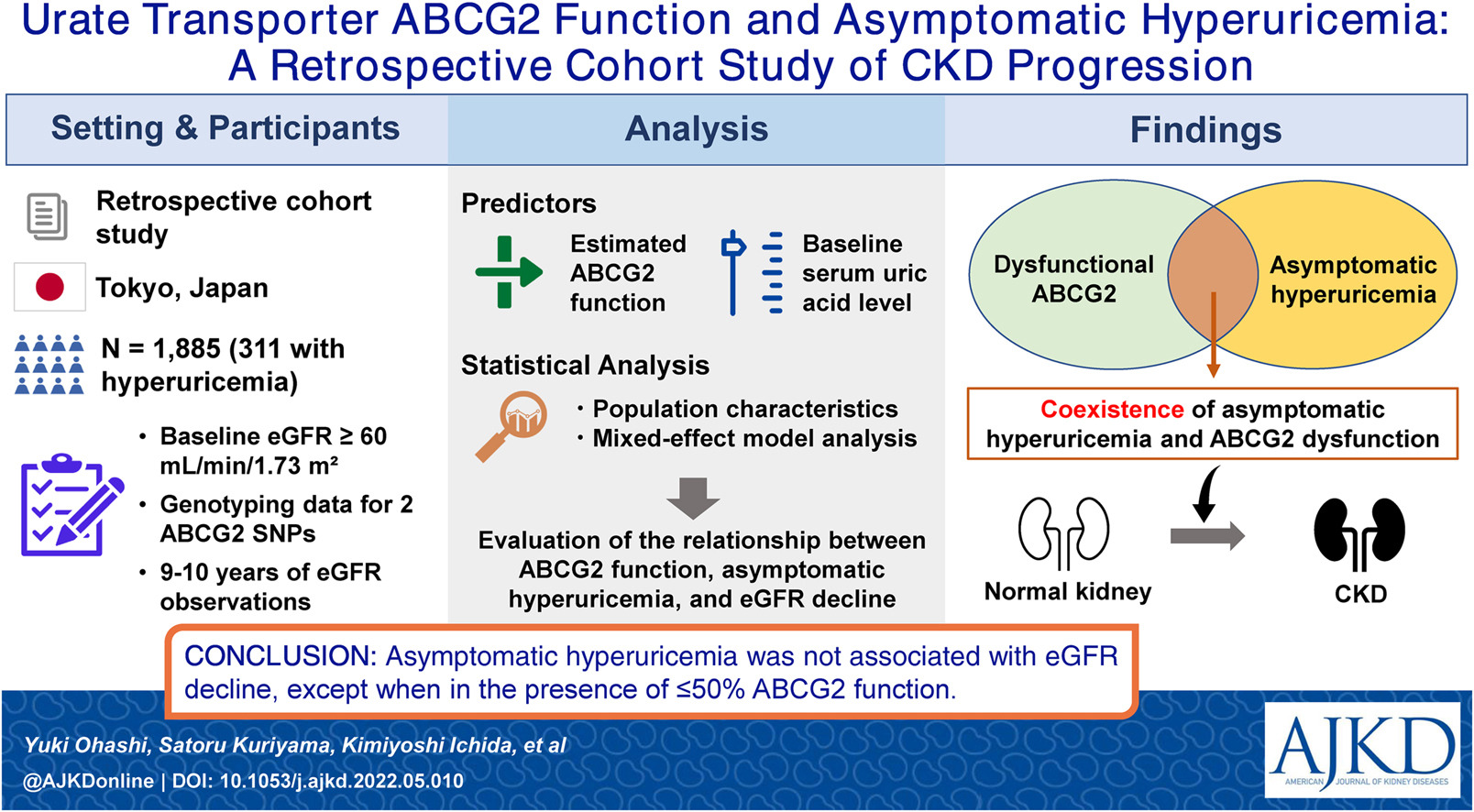
Urate Transporter ABCG2 Function and Asymptomatic Hyperuricemia: A Retrospective Cohort Study of CKD Progression by Yuki Ohashi et al
From the authors: The urate transporter ABCG2 is a protein that regulates serum urate concentrations; when dysfunctional, it can lead to elevated serum concentrations of this compound (ie, hyperuricemia). Although persistent hyperuricemia induces gout and kidney injury, the effects on organs during the asymptomatic phase have yet to be established. Therefore, to clarify the relationship between ABCG2, asymptomatic hyperuricemia, and kidney function, we conducted a retrospective cohort study of 1,885 healthy participants, including 311 participants with asymptomatic hyperuricemia. We found that the coexistence of asymptomatic hyperuricemia and severe ABCG2 dysfunction was associated with the age-dependent decline in kidney function. We concluded that asymptomatic hyperuricemia represents a risk factor for chronic kidney disease, at least in individuals with highly dysfunctional ABCG2. This new finding highlights the potential importance of ABCG2 in the pathogenesis of hyperuricemia-induced kidney injury.
DOI: 10.1053/j.ajkd.2022.05.010
Editorial: Intestinal Hyperuricemia as a Driving Mechanism for CKD by Richard J. Johnson [FREE]
Lumasiran for Advanced Primary Hyperoxaluria Type 1: Phase 3 ILLUMINATE-C Trial by Mini Michael et al [OPEN ACCESS]
From the authors: Primary hyperoxaluria type 1 (PH1) is a rare genetic disease characterized by excessive hepatic oxalate production that frequently causes kidney failure. Lumasiran is an RNA interference therapeutic that is administered subcutaneously for the treatment of PH1. Lumasiran has been shown to reduce oxalate levels in the urine and plasma of patients with PH1 who have relatively preserved kidney function. In the ILLUMINATE-C study, the efficacy and safety of lumasiran were evaluated in patients with PH1 and advanced kidney disease, including a cohort of patients undergoing hemodialysis. During the 6-month primary analysis period, lumasiran resulted in substantial reductions in plasma oxalate with acceptable safety in patients with PH1 complicated by advanced kidney disease.
DOI: 10.1053/j.ajkd.2022.05.012
Editorial: Primary Hyperoxaluria: A Need for New Perspectives in an Era of New Therapies by Michael J.G. Somers [FREE]
Sex Disparity in Cause-Specific and All-Cause Mortality Among Incident Dialysis Patients by Wai H. Lim et al
Supermarket Proximity and Risk of Hypertension, Diabetes, and CKD: A Retrospective Cohort Study by Gaurang Garg et al
From the authors: Residing in an environment with limited access to healthy food may be a modifiable risk factor for the development of hypertension, diabetes, and kidney disease. We used a household’s distance to the closest supermarket as a measure of food access and calculated the average distance to the nearest supermarket for 56 Chicago zip codes. We also calculated the incidence of hypertension, diabetes, and kidney disease for each of those zip codes using electronic health data. We found that supermarket distance is a confounding marker for a number of other important individual factors like race, sex, and age and neighborhood factors like income, racial composition, and access to a vehicle. Changing disparities in chronic diseases will require broad, multifaceted solutions.
DOI: 10.1053/j.ajkd.2022.07.008
Peritoneal Dialysis–Associated Peritonitis Trends Using Medicare Claims Data, 2013-2017 by Eric W. Young et al
From the authors: Peritonitis is an important complication that affects peritoneal dialysis patients. We used claims information in US registry data to identify peritonitis episodes. We identified diagnoses that are associated with peritonitis and developed rules for handling ambiguous data, such as “clusters” of peritonitis-indicting diagnoses that might belong to 1 or more episodes. Our approach identified consistent differences in the risk of peritonitis by race and by age, and a substantial drop in the peritonitis rate over time. This approach highlights the need for uniform coding standards for peritonitis and could be used to help identify additional risk factors and opportunities to improve clinical practice.
DOI: 10.1053/j.ajkd.2022.07.010
Plasma Soluble Tumor Necrosis Factor Receptor Concentrations and Clinical Events After Hospitalization: Findings From the ASSESS-AKI and ARID Studies by Steven G. Coca et al
From the authors: Two proteins linked to proinflammatory cell signaling pathways, sTNFR1 and sTNFR2, are associated with kidney-related outcomes in patients with chronic kidney disease with and without diabetes. However, whether their levels can predict events occurring after a hospitalization is unknown. We found that high levels of sTNFR1 and sTNFR2 measured 3 months after hospital discharge are associated with kidney disease–related events, heart failure hospitalizations, and death among patients who did and did not have acute kidney injury during the hospitalization. Furthermore, the sTNFR proteins provide discriminative value at the time of predicting kidney events. These findings were demonstrated in 2 large independent prospective cohorts. Measuring sTNFR1 and sTNFR2 may help in detecting patients at risk of future adverse events even when patients do not meet the clinical criteria for acute kidney injury or exhibit biochemical abnormalities.
DOI: 10.1053/j.ajkd.2022.08.007
Anemia Prevalence, Type, and Associated Risks in a Cohort of 5.0 Million Insured Patients in the United States by Level of Kidney Function by Danielle K. Farrington et al
From the authors: Anemia, a common complication of chronic kidney disease, is associated with adverse outcomes. Unfortunately, the use of erythropoiesis-stimulating agents (ESAs) to target a normal hemoglobin level has been associated with increased cardiovascular risk. Our large study of over 5 million patients sought to describe the burden and risk factors associated with anemia by level of kidney function. We found that severe anemia was common and strongly associated with lower kidney function and multiple adverse outcomes. ESA use was rare. Although iron levels were checked infrequently, low iron test results were common in those tested. This highlights the need for increased testing of iron level in patients with anemia, as iron supplementation is an effective and low-risk intervention.
A National Registry for People With All Stages of Kidney Disease: The National Kidney Foundation (NKF) Patient Network by Lesley A. Inker et al [FREE]
From the authors: The NKF Patient Network (NKFPatientNetwork.org) is a nationwide kidney disease patient registry created to improve the lives of people with kidney disease through research, clinical care, and drug development. The Network has a secure portal for participants to share their experiences and data, and for providers to upload electronic health records with patient consent. The Network also offers individualized education and support. In this feasibility study, we found low awareness of kidney disease for many participants and a challenge in recruiting vulnerable populations. Overcoming both of these difficulties are short-term goals of the Network following the national launch in February 2021. Overall, the Network will facilitate real-world data collection to inform the development of patient-centered research, care, and treatments for people with kidney disease.
Deceased-Donor Acute Kidney Injury and Acute Rejection in Kidney Transplant Recipients: A Multicenter Cohort by Peter P. Reese et al [OPEN ACCESS]
From the authors: Many patients in the United States wait years for a kidney transplant because of a shortage of good-quality donated kidneys. One way to relieve this problem is to transplant kidneys that experienced inflammation and injury in the deceased donor before transplant. We measured the level of kidney injury in the urine of 862 donors. We then studied the clinical outcomes for the 1,137 adult recipients of kidneys transplanted from those donors. Compared with recipients of kidneys from donors with less injury, the recipients of injured kidney transplants did not experience higher rates of a combined outcome of rejection or failure of the transplant. These results provide evidence that transplant centers can successfully manage transplantation using injured kidneys from deceased donors.
Review from the February 2023 issue:
Calciphylaxis and Kidney Disease: A Review by Benjamin Marin et al (FREE)
Calciphylaxis is a life-threatening complication most often associated with chronic kidney disease that occurs as a result of the deposition of calcium in dermal and adipose microvasculature. However, this condition may also be seen in patients with acute kidney injury. The high morbidity and mortality rates associated with calciphylaxis highlight the importance to correctly diagnose and treat this condition. However, calciphylaxis remains a diagnosis that may be clinically challenging to make. The authors review the literature on uremic calciphylaxis with a focus on its pathophysiology, clinical presentation, advances in diagnostic tools, and treatment strategies. They also discuss the unique histopathological features of calciphylaxis and contrast it with those of other forms of general vessel calcification. This review emphasizes the need for multidisciplinary collaboration including nephrology, dermatology, and palliative care to ultimately provide the best possible care to patients with calciphylaxis.
DOI: 10.1053/j.ajkd.2022.06.011
 On the Cover: AJKD is honored to present the 11th annual NephMadness, organized by Executive Team members Matthew Sparks, Timothy Yau, Anna Burgner, Samira Farouk, Pascale Khairallah, and Anna Vinnikova. This educational initiative highlights 8 important nephrology topics and encourages participants to select the one most likely to change kidney disease care in the next 5 years. US-based physicians can claim up to 8.0 CME credits and MOC points for this activity. The fun and learning will begin on March 1, 2023, at http://www.AJKDBlog.org.
On the Cover: AJKD is honored to present the 11th annual NephMadness, organized by Executive Team members Matthew Sparks, Timothy Yau, Anna Burgner, Samira Farouk, Pascale Khairallah, and Anna Vinnikova. This educational initiative highlights 8 important nephrology topics and encourages participants to select the one most likely to change kidney disease care in the next 5 years. US-based physicians can claim up to 8.0 CME credits and MOC points for this activity. The fun and learning will begin on March 1, 2023, at http://www.AJKDBlog.org.
The NephMadness 2023 logo is created by Graham T. Gipson, AJKD






Leave a Reply