#NephMadness 2023: Ready to Rumble
Submit your picks! | NephMadness 2023 | #NephMadness | #OncoNephrology
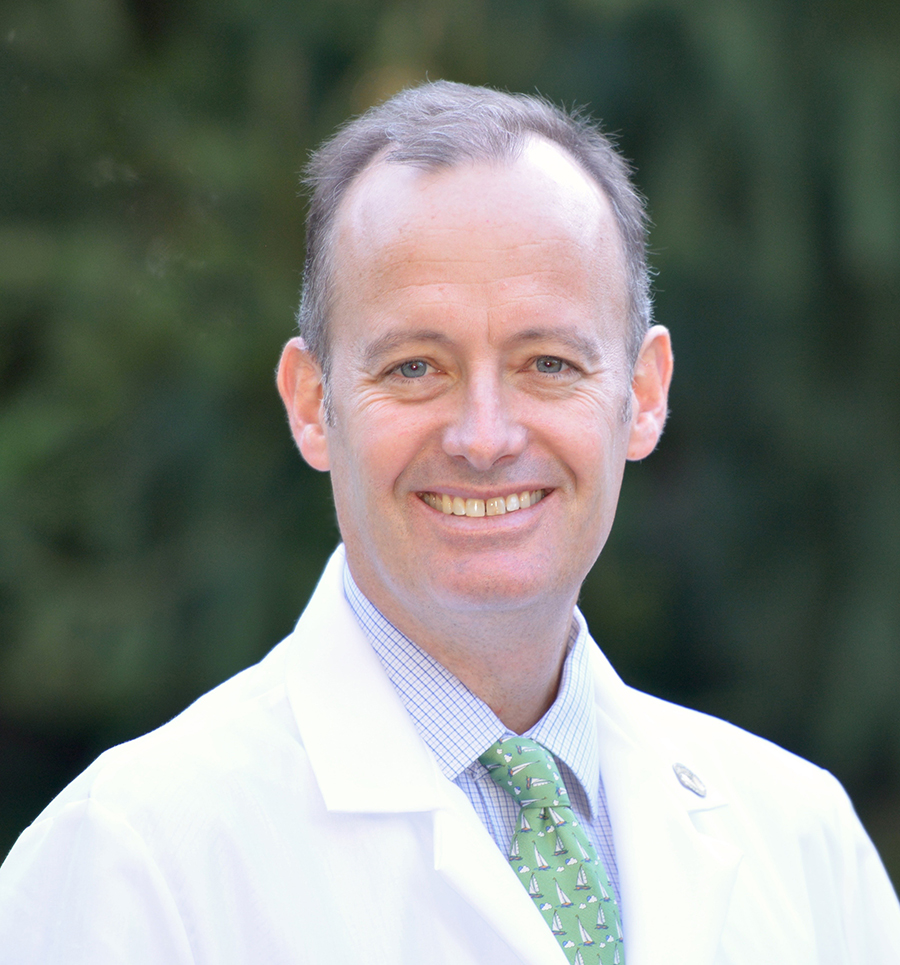
Ben Humphreys @HumphreysLab
Dr. Humphreys is Chief of the Division of Nephrology and the Joseph Friedman Professor at Washington University in St. Louis as well as President-elect for the American Society of Clinical Investigation. His research focuses on kidney injury and fibrosis using single cell multi-omics and spatial transcriptomics as approaches. He has a clinical interest in onco-nephrology.
Competitors for the Onconephrology Region
Chemotherapy-Associated Hypomagnesemia vs Immune Checkpoint Inhibitor-Associated Acute Kidney Injury

Copyright: Antoine2K/Shutterstock
The onconephrology matchup this year features two heavyweights: EGFRi-induced hypomagnesemia vs. ICI-induced AKI. If this were a boxing match, it would be the precision of Muhammed Ali (“Float like a butterfly, sting like a bee”) vs. the power of Mike Tyson (“Everyone has a plan until they get punched in the mouth”). If these were digital tools, EGFRi’s are a hypersegmented facebook precision advertising campaign and ICIs are an email spam filter that keeps unwanted emails out but sometimes blocks your friends and family too.
This year’s contest reflects the growing depth and maturity of the onconephrology subspecialty itself. In one corner, we have a highly accurate, targeted therapy – anti-EGFR inhibitors – that exerts anticancer effects by inhibiting a signaling pathway that some tumors require for survival and expansion. But these drugs are both specific and highly potent, so toxicities result from inhibition of the same biologic pathway in a non-cancer tissue, where the pathway regulates some aspect of organ homeostasis. As eloquently described by Stockholm and Schoer, inhibition of basolateral EGFR in the distal tubule suppresses the magnesium channel TRPM6, causing magnesium wasting and hypomagnesemia.

Copyright: Wooden Owl/Shutterstock
What other examples of “on-target” toxicities exist in onco-nephrology? Antiangiogenic therapies target the vascular endothelial growth factor (VEGF) molecule, its receptor or downstream pathways. FDA approved antiangiogenic agents include bevacizumab, a recombinant, humanized monoclonal antibody that binds and sequesters the VEGF molecule, and multi-targeted tyrosine kinase inhibitors (TKI), small molecules that inhibit the VEGFR intracellular intrinsic kinase activity, such as sunitinib, sorafenib, axitinib and pazopanib. Antiangiogenic therapies are first line therapy for cancers such as metastatic renal cell carcinoma and they act by inhibiting tumor-induced angiogenesis – effectively starving the cancer of needed oxygen and nutrients.
Anti-angiogenic therapies can cause proteinuria that is most commonly the consequence of renal thrombotic microangiopathy (TMA). The clinical syndrome is characterized by hypertension, microangiopathic hemolysis, kidney injury, sub-nephrotic proteinuria and microscopic hematuria. On kidney biopsy, endotheliosis is the most prominent feature, and endothelial injury is reflected by thickened basement membranes with double contours. The pathophysiology of this syndrome involves VEGF expressed by podocytes and blockade of the VEGF signal on glomerular endothelial cells. Eremina, et al. elegantly recapitulated a renal limited TMA in mice by ablating VEGF from podocytes alone. Thus, antiangiogenic therapies act by blocking the effect of podocyte-derived VEGF on adjacent glomerular endothelial cells, resulting in disruption of the glomerular filtration barrier with proteinuria, as well as enhanced clotting.
What these toxicities reveal – both EGFRi-induced hypomagnesemia – and antiangiogenic therapy-induced TMA – is how the toxicities of targeted therapies in the modern era can help us understand human biology by revealing unanticipated roles for the signaling pathways these drug block in kidney homeostasis.
The lessons of ICI for onconephrology are quite distinct from EGFRi. While technically also a targeted therapy, the consequences of ICI are to unleash the full power of the human immune system in a much less predictable way. The anticancer effects of this drug class are remarkable but immune-related adverse events (irAE’s) are common; we do not fully understand their pathogenesis and they pose challenges in clinical management. In this sense the experience we have gained concerning ICI-related AKI over the last decade reflects the real-world generation of new medical knowledge initially through observation and trial and error and later through careful investigation with larger and larger patient cohorts.
Copyright: Grigvovan/Shutterstock
While we have come a long way in understanding the kidney effects of ICI, many important and fascinating questions remain. If acute tubulointerstital nephritis (ATIN) is the most common pathology caused by ICI, how common are other glomerular injury patterns, and what are the risk factors for their development? How safe is it to rechallenge patients with ICI after a kidney complication from the therapy? Are we not biopsying enough, or biopsying too much? Are ICI safe in transplant recipients? These are all important questions that are outlined by the region and require further investigation in order to generate evidence-based guidelines to achieve the best outcomes for our patients.
It is hard to call a winner in this onconephrology veteran bout. After 12 rounds, ICI-induced AKI takes the win (in a split decision) for exemplifying the way that a new class of cancer therapy can force the onconephrology community to come together, gather data, test hypotheses and ultimately advance medical science.
– Guest Post written by Ben Humphreys @HumphreysLab
As with all content on the AJKD Blog, the opinions expressed are those of the author of each post, and are not necessarily shared or endorsed by the AJKD Blog, AJKD, the National Kidney Foundation, Elsevier, or any other entity unless explicitly stated.
Click to read the Onconephrology Region
Submit your picks! | #NephMadness | @NephMadness | #OncoNephrology

Leave a Reply