Itching for Answers: Associations of CKD-Associated Pruritus with Adverse Health Outcomes
Dr. Kayla Caruso is a Palliative Medicine fellow at the University of New Mexico. She enjoys seeing patients in the outpatient and inpatient settings to discuss what matters most and collaborating with primary and specialty providers to address symptoms and improve wellbeing.
Dr. Sara Combs is a Nephrologist and Palliative Medicine physician and serves as the Program Director for Internal Medicine residency at the University of New Mexico. Dr. Combs is passionate about improving the quality of life of patients with chronic kidney disease and loves teaching about all things related to symptoms they experience, especially CKD-associated pruritus.
Symptom burden in patients with chronic kidney disease (CKD) greatly affects patients’ quality of life. Adequate symptom management is a cornerstone of patient-centered care. Pruritus is one of the most bothersome symptoms experienced by patients with advanced chronic kidney disease. Patients with advanced kidney failure have named treatment of pruritus as a top research priority. Yet the literature supports that nephrologists and other health care providers underestimate its prevalence, severity, and significance. Patients also underreport the symptom to their providers, presumably because they may not be asked about it or because they perceive that there may not be effective treatment, and unsurprisingly, patients report that their CKD-associated pruritus (CKD-aP) is inadequately treated.
The presentation of CKD-aP is variable, but frequently presents as itching that affects large, discontinuous but bilateral and symmetrical areas of skin. It is often persistent, generalized, and commonly affects the back, abdomen, arms, legs, and scalp. Patients may have targeted pruritus as well, such as on or near their hemodialysis access site. Precipitating factors commonly include heat, dialysis, stress, cold, physical activity, showering, and rest or sleep. On exam, there are no visible skin findings other than excoriations or scarring that occur due to persistent scratching.
There are validated and easy-to-use assessment tools for CKD-aP that can help providers identify patients suffering from the symptom and assess response to treatment. The Worst Itching Intensive Numeric Rating Scale, for example, is an easy tool that can help assess patient response to treatment, with a reduction of 3 or greater on this scale representing a clinically meaningful improvement in itch.
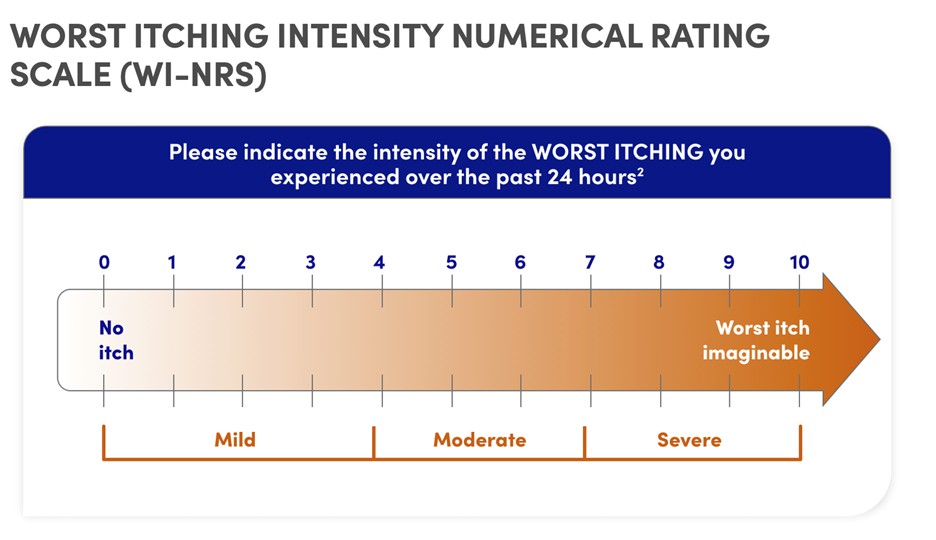
The Worst Itching Intensity Numerical Rating Scale Based on Figure S1 from Vernon et al, Creative Commons Attribution 4.0 International License.
Data supporting treatment options are generally hampered by small sample size and methodologic limitations. A step-by step treatment approach using topical therapies, gabapentinoids, and opioid-receptor modulators is recommended by expert guidelines. Despite the availability of these guidelines, providers frequently recommend treatments that have not been shown to be effective and often prescribe medications (such as antihistamines) that can be harmful.
In a study recently published by Faucon et al. in AJKD that sought to quantify the burden of CKD-aP and its associated adverse health outcomes in a Swedish population, the authors took a novel approach to identify cases of pruritus. Using data from the Swedish Renal Registry, this study defined clinically recognized pruritus by “the presence of a [ICD-10] clinical diagnosis in the patient medical records, the chronic use of pruritus medications, and/or the use of UV therapy (in the absence of a diagnosis of psoriasis).” During the study interval of 2005-2021, nephrologists in Sweden managed CKD-associated pruritus with treatments including hydroxyzine, clemastine, gabapentin, pregabalin, and a compounded topical preparation classically known as klådsalva in Swedish (meaning “ointment for itching”).
Among the 3,281 identified patients receiving maintenance dialysis, 14% had pruritus at enrollment and during a median follow-up of 3.3 years, 19% additional patients experienced pruritus. Patients with pruritus, whether pre-existing or new-onset, were at a higher risk of sleep disorders, developing new-onset anxiety/depression, and being hospitalized for severe infections. Researchers attributed these infections to an increased risk of sepsis and peritoneal dialysis–related peritonitis. Though they did not find an association between the development of pruritus and all-cause mortality, there were independent associations between pruritis and older age, female sex, a lower serum albumin level, and higher levels of C-reactive protein, serum calcium, and phosphorus.
The total prevalence of 33% of patients that experience pruritus during their first years receiving maintenance dialysis in this study is consistent with other data. In the DOPPS cohort, the prevalence of Swedish patients who self-reported being moderately to extremely bothered by pruritus as assessed by the question, “During the past 4 weeks, to what extent were you bothered by: itchy skin?”, was 37%. One would guess that using a clinical measure rather than a patient assessment tool to quantify a symptom would greatly underestimate symptom prevalence, especially given that we know that healthcare providers underrecognize CKD-aP. In this recent AJKD study, 36% of cases were identified through ICD-10 codes and 64% through initiation of a treatment. This may suggest that providers often prescribe treatments for “itch” without recognizing or identifying the etiology or pathophysiology for the pruritus (to a level, at least, that they document a chart diagnosis). At a minimum, it seems that it could be concluded that documentation of symptoms is not a priority for providers or the system in which they work, leaving us to reflect on how the healthcare system could better support prioritization of patients’ symptoms and quality of life and how that might improve patient care.
Both the prevalence of CKD-aP in patients receiving hemodialysis and its associations with impaired quality of life are already very well-established in the literature.
While fundamentally these observational results still can only be used to imply rather than prove causation, the temporal relationship observed in this study between the onset of pruritus and a decrement in quality of life goes beyond prior studies in helping establish a causative link between pruritus and impaired quality of life in patients with kidney failure. It is interesting that there was not a significant association measured between mortality and CKD-aP, in contrast to many other studies. Regardless, the impact of CKD-aP on patients’ quality of life is undeniable. It should be noted that DOPPS (a much larger cohort) did not find an association between CKD-aP and serum phosphate nor calcium, and in this study the adjusted odds or hazard (depending on prevalent or new-onset pruritus) of phosphate and calcium were minimal (1.06 and 1.12 and 1.11 and 1.08, respectively). Treatment for CKD-aP often focuses on mineral bone disease metrics, where patients are blamed for non-adherence to treatments and frequently told that their symptom of itch will improve should their phosphate values improve. Rather, there are easy-to-use guidelines for providers to use to ensure that patients are offered effective treatments for their CKD-aP, and it’s time we feel empowered to use them.
-Post prepared by Kayla Caruso and Sara Combs
To view Faucon et al (Open Access), please visit AJKD.org:
Title: Burden of CKD-Associated Pruritus and Adverse Clinical Outcomes in Patients Receiving Dialysis: The Stockholm Creatinine Measurements (SCREAM) Project
Authors: Anne-Laure Faucon, Catherine M. Clase, Helena Rydell, Milica Uhde, Peter Barany, Marie Evans, Juan-Jesús Carrero
DOI: 10.1053/j.ajkd.2024.05.013



Leave a Reply