Advanced Age Living Kidney Donation: How Old is Too Old?
Dr. Akshta Pai, MD, MPH is an Assistant Professor at the Donald and Barbara Zucker School of Medicine at Hofstra. She is the Director of Strategic Development and Outreach for kidney transplantation at Northwell Health Transplant Institute where she is engaged in increasing access to transplantation.
The dawn of kidney transplantation began with the first successful living donation in 1954 between twin brothers. However, the early years were fraught with challenges. Unsuccessful outcomes among recipients with non-identical donors led to a temporary discouragement of living donation. Fast forward to now, 70 years later, where we not only encourage living donation from all donors, but we are contemplating how old is too old to be a living donor.
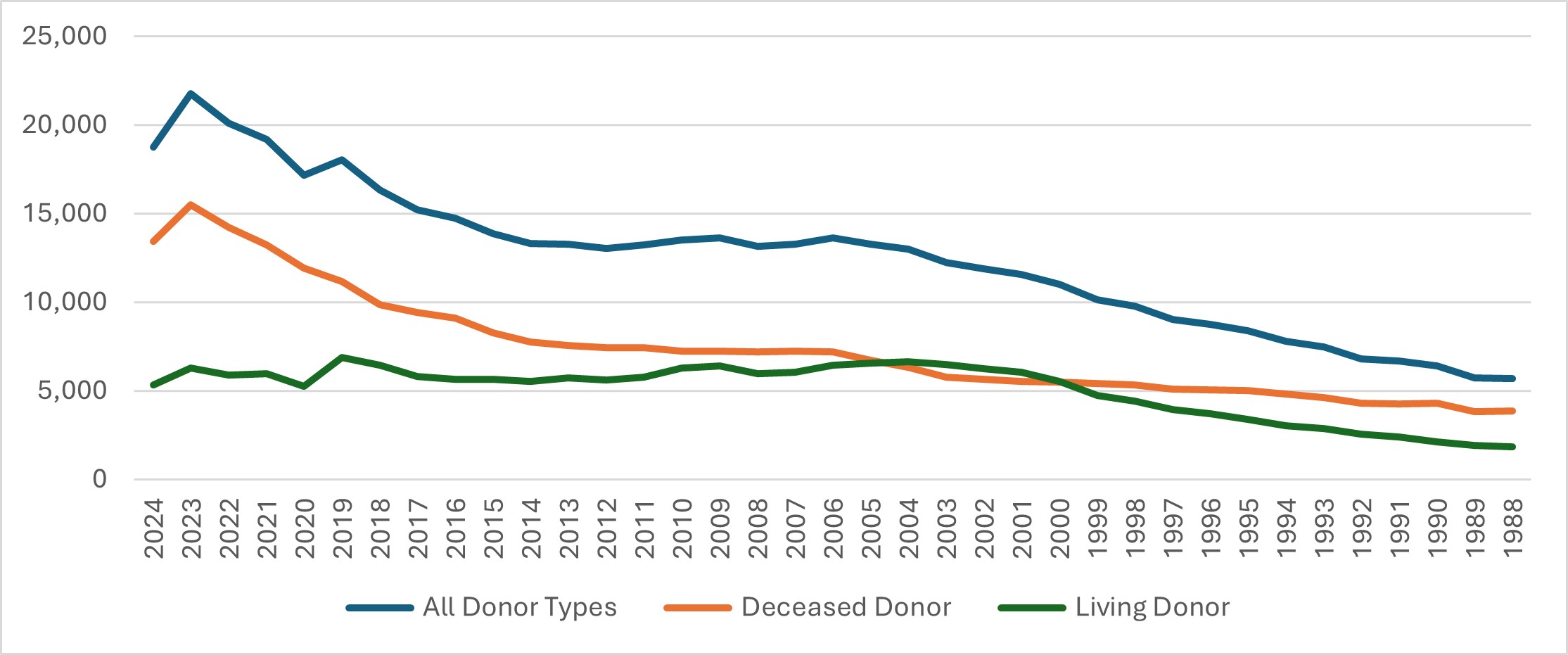
Expanding the donor pool remains a key challenge in reducing kidney transplant waiting times, seen as stagnant transplant rates among recipients on dialysis (Figure 1). While xenotransplantation has generated excitement within the transplant community, its large-scale feasibility remains distant. Although the availability of deceased donor kidneys has increased, living donation has declined over the past decades (Figure 2), making efforts to boost it a priority. One significant obstacle is the lack of comprehensive long-term follow-up data on living donors. The transplant community has worked to gather and report data on living donors, leveraging multiple datasets to generate valuable but inherently limited observational evidence.
A recent study contributing to this growing body of research is Medical Suitability and Willingness for Living Kidney Donation Among Older Adults by Villain et al. Using data from the Berlin Initiative Study (BIS), the study examines how long older adults remain eligible as kidney donors and how their willingness to donate changes over time. The BIS, conducted from 2009 to 2019, followed 2,069 participants from Berlin’s largest health insurance fund to track kidney function in individuals over 70 years old. It collected data through face-to-face questionnaires, along with blood and urine samples. Villain et al. conducted a secondary analysis of BIS data, applying medical criteria from KDIGO and the British Transplant Society (BTS) to assess donor eligibility, while also incorporating an additional questionnaire to evaluate participants’ willingness to donate.
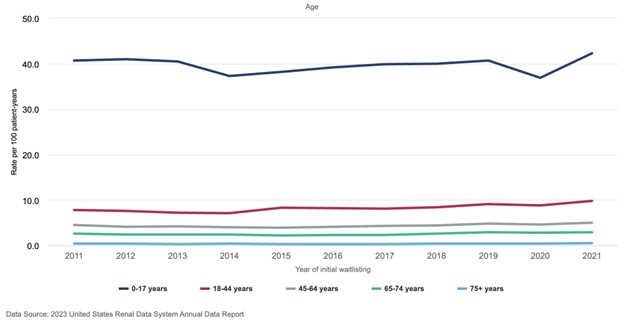
Figure 1. Rate (per 100 person-years) of kidney transplants by recipient age in patients undergoing dialysis (2011-2021)Figure 7.10b from United States Renal Data System. 2023 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2023.
KDIGO and the British Transplant Society (BTS) have established standard guidelines for medically suitable living kidney donors based on existing data. Both organizations recommend a baseline glomerular filtration rate (GFR) of 80–90 mL/min in donors, with an absolute contraindication for transplantation if GFR falls below 45–60 mL/min. A key challenge in this study was that no participant had a Cr/CysC GFR of 90 mL/min. The median GFR at baseline was 63 mL/min, with a median age of 80.4 years. Based on GFR, proteinuria, and medical comorbidities, only 5% of participants met the criteria for medical suitability. These individuals were more likely to be younger (70–79 years vs. 80+ years), female, married, and reported better overall health. Among those initially deemed suitable, 42–46% remained eligible after two years, but this percentage dropped to just 11–16% at eight years. Most participants lost eligibility due to the development of non-kidney medical comorbidities, while 11–12% progressed to chronic kidney disease (CKD) within two years, leading to exclusion. However, those who remained suitable at eight years did not develop CKD. Over the course of the study, mortality ranged from 6–11%. Encouragingly, 80–85% of suitable candidates were willing to donate, compared to lower willingness among those deemed unsuitable. Older participants (80+ years) were generally less willing to donate a kidney.
This study offers valuable insight into the challenges and possibilities of older adults as potential kidney donors. While most do not meet the criteria due to medical comorbidities, those who do tend to be younger (<80 years), female, and married. In prioritizing non-maleficence, particularly for older donors, this study underscores the importance of identifying an optimal timing for donation among suitable candidates. Although the study briefly mentions the cost of donor evaluations, it does not provide comparisons to other donor types, discuss potential financial implications post-donation, or offer a comprehensive cost-benefit analysis. Despite these gaps, the findings reinforce the need to apply existing donor selection guidelines with careful consideration. While a significant expansion of the donor pool among older adults may be medically limited, individualized assessments remain crucial. Additionally, the study suggests that rigid age cutoffs could be unnecessarily restrictive.
The Living Donor Collective (LDC), a pilot program launched around 2017 to establish a national living donor registry, is a long-term data collection program. LDC currently has a short follow-up period, but it provides valuable insights into the donor evaluation process, including data on candidates who were not approved and the reasons for their rejection. Notably, the findings of Villain et al. align with trends observed in the LDC, where the lowest percentage of approved donors were aged 65 and older, while women and those in partnered relationships were more likely to be approved. Interestingly, approval rates were nearly nonexistent for individuals with a GFR below 60 mL/min. However, those with a GFR between 60–90 mL/min were approved at a higher rate than those with a GFR above 90 mL/min.
The transplant community needs more detailed pre- and post-donation follow-up to validate the observations seen in studies like Villain et al., further informing best practices for living donor selection and long-term outcomes.
-Post prepared by Akshta Pai
To view Villain et al, please visit AJKD.org:
Title: Medical Suitability and Willingness for Living Kidney Donation Among Older Adults
Authors: Cédric Villain, Natalie Ebert, Richard J. Glassock, Nina Mielke, Tim Bothe, Muhammad Helmi Barghouth, Anna Pöhlmann, Anne-Katrin Fietz, John S. Gill5, Elke Schaeffner
DOI: 10.1053/j.ajkd.2024.07.010


Leave a Reply