Renal Denervation: Are We There Yet?
Edgar Lerma @edgarvlermamd
Dr. Edgar Lerma is a clinical nephrologist practicing in the south suburbs of Chicago. He holds the rank of Clinical Professor of Medicine at the University of Illinois at Chicago (UIC) and serves as Educational Coordinator for the section of Nephrology with the Internal Medicine Residency Training Program at Advocate Christ Medical Center in Oak Lawn, IL. He is a member of the American Board of Internal Medicine (ABIM) Approval Committee and is the KDIGO Knowledge Translation Lead. Aside from his teaching and educational involvement, he is also active on social media and was an AJKD Blog Contributor from 2013-2022.
Sherida Edding @ShedaEdding
Dr. Edding is currently in her 3rd year of Internal Medicine residency at Lincoln Medical Center, The Bronx, NY. She is an aspiring Nephrologist and is busy with the fellowship process this season. She has an interest in Renal Transplantation and medical education through social media. She was a member of NephSIM 2021 and 2022. She contributed her first AJKD blog article last May 2022.
Angel Ortiz @AngelCesarOrtiz
Dr. Angel Ortiz is currently chief of the department of internal medicine at IMSS, Queretaro. He is a nephrologist and obtained a Master of medical investigation from Universidad Autonoma de Queretaro. He completed his residency at the Universidad Nacional Autonoma de Mexico. He was part of the International Society of Nephrology Social Media team. His research interests include dialysis in elderly and glomerular disorders. He enjoys hiking, travelling and medical education.
Hypertension (HTN) is a major risk factor for cardiovascular and renal disease. The 2021 KDIGO guidelines recommend that the systolic blood pressure target for adult patients with chronic kidney disease (CKD) should be a systolic blood pressure (SBP) of less than 120 mm Hg. The combination of lifestyle modifications and antihypertensive drug regimens has been the cornerstone of treatment to date.
Resistant HTN is defined as a blood pressure that remains above goal despite concurrent use of three antihypertensive agents of different classes taken at maximally tolerated doses, one of which being a diuretic. Resistant HTN remains a clinical challenge for both physician and patient.
The search for more effective ways to manage hypertension, particularly resistant hypertension calls for revisiting renal denervation as a potential therapy. In their comprehensive review article, Rey and Townsend outline the different mechanisms of denervation, its efficacy, safety and challenges across different patient populations, and the ongoing work in this rapidly developing field.
What exactly is renal denervation? Nerves extend from the sympathetic ganglia and travel along the renal artery (and side branches) innervating the kidneys. Renal denervation aims to ablate the nerves reaching the kidneys, thereby interrupting the sympathetic tone. The sympathetic system is targeted because when stimulated it leads to increased renin release, reduction in sodium excretion and increased renal vascular resistance.
Renal denervation can be accomplished using three different approaches – radiofrequency ablation (RFA), ultrasound-guided (US) ablation or via injection of a neurotoxin (Table 1). Click this link to see how RFA is performed and this link for a brief video of US-guided RDN.
Initial renal denervation studies showed a 25-30 mm Hg reduction in the systolic blood pressures of patients who had office systolic blood pressure readings of greater than 160 mm Hg and were on 5 or more antihypertensives. However, later sham-controlled trials had similar office blood pressure reductions in both the renal denervation and the sham groups. These findings led to skepticism regarding renal denervation and its antihypertensive effect.
However, better knowledge of the kidney nerve anatomy and improvement in techniques led to some better results. In subjects with uncontrolled HTN, studies such as SOLO (visual abstract 1), SPYRAL HTN-ON (visual abstract 2) and SPYRAL HTN-OFF (visual abstract 3) showed that renal denervation can decrease the systolic blood pressure by 9 mm Hg.

Visual Abstract 1. RADIANCE-HTN SOLO, Azizi M, et al., The Lancet

Visual abstract 2. SPYRAL HTN-ON, Kandzari DE, et al. The Lancet

Visual abstract 3. SPRYAL HTN-OFF, Townsend R, et al., The Lancet
In patients with chronic kidney disease, renal denervation showed a trend towards decreasing blood pressure without a negative effect on eGFR. Few smaller studies noted stabilization or even improvement in eGFR after renal denervation. Of note, studies have excluded patients with eGFR <45 mL/min/1.73 m2.
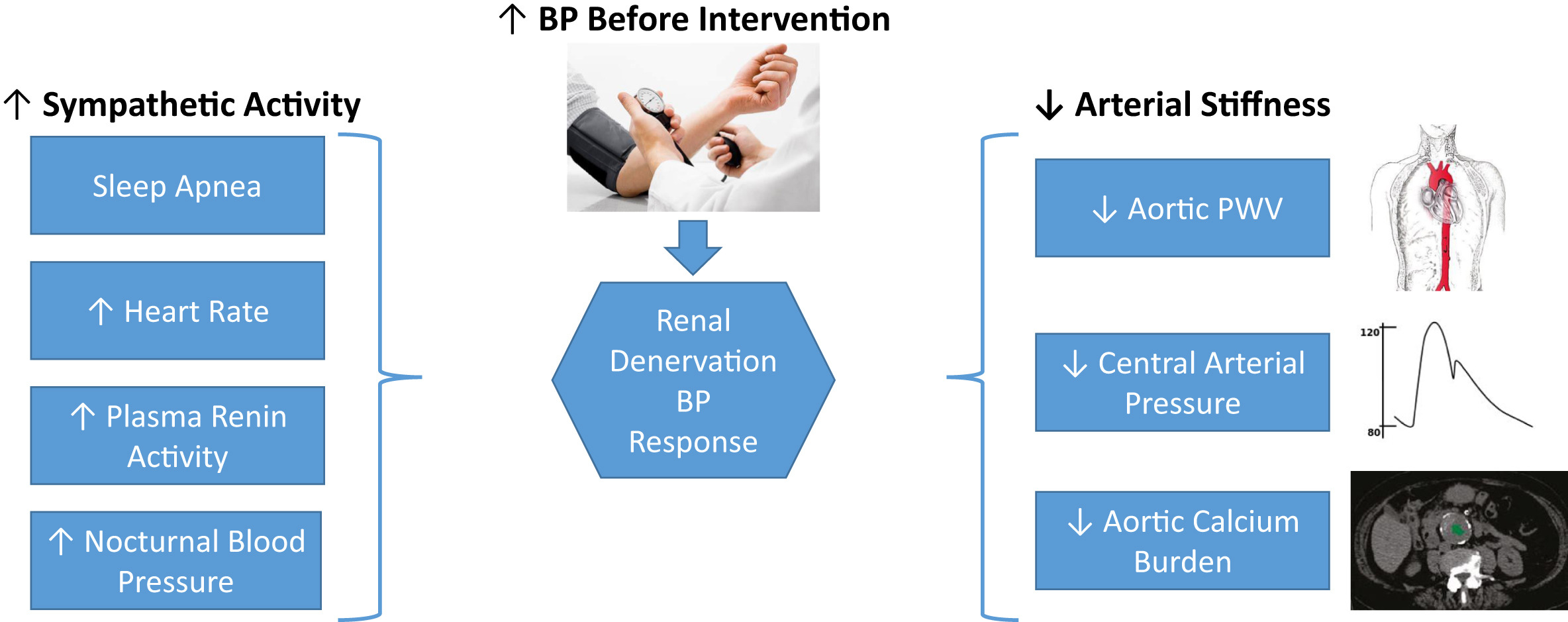
Predictors of renal denervation (RDN) response. Figure 4 from Rey and Townsend, AJKD © National Kidney Foundation.
In addition to the blood pressure effect, subgroup analyses of diabetic patients enrolled in renal denervation trials suggest that renal denervation may decrease fasting blood glucose and improve insulin sensitivity.
Despite some benefits to renal denervation, there remain several roadblocks to its implementation in clinical practice:
- patients should be willing to undergo a procedure with potential risks (including renal artery stenosis)
- physicians should be willing to refer patients to such intervention and consider it a tool in their blood pressure management armamentarium
More renal denervation clinical trials are in the pipeline and their results should give us more definitive answers regarding renal denervation’s benefits.
–Post prepared by Sherida N. Edding and Edgar V. Lerma. Visual Abstracts by Angel Ortiz.
To view Rey et al (FREE), please visit AJKD.org.
Title: Renal Denervation: A Review
Authors: Jimena Ray and Raymond R. Townsend
DOI: 10.1053/j.ajkd.2022.03.015


Leave a Reply