Toward a Successful Shared-Care Model for Kidney Transplant Recipients
Deborah Lee, MD, is a second year nephrology fellow at University of California San Francisco. She completed her medical education at the Indiana University School of Medicine, and her internal medicine residency at Virginia Mason Medical Center in Seattle. She plans to pursue a career in transplant nephrology.
Pascale Khairallah, MD, MS, is a transplant nephrologist and Assistant Professor of Medicine at the University of California, San Francisco. Her clinical and research interests focus on bone and mineral metabolism, cardiovascular risk, and long-term outcomes after kidney transplantation. She also serves as the editor for the AJKD Blog Commentary series.
Kidney transplantation remains the optimal therapy for kidney failure, improving quality of life and survival compared with dialysis. As transplant outcomes have improved and patient survival has lengthened, the population of individuals living with a functioning allograft has grown and continues to grow yearly. In 2024 alone, Centers for Medicare & Medicaid Services (CMS) reported that approximately 28,000 kidney transplants were performed, and that more than 80,000 new patients were added to the transplant waitlist. However, the transplant nephrology workforce remains very limited with only 800-1000 transplant nephrologists across the United States. This translates into roughly one transplant nephrologist for every 300 kidney transplant recipients, not accounting for the burden of managing the waitlist which also falls heavily on transplant nephrologists. This highlights a dual challenge: growing transplant demand on one side, and a limited transplant nephrology workforce on the other.
In current practice, most transplant centers refer stable recipients back to their referring nephrologists after the first-year post-transplantation. Yet, patients with unstable or poor allograft function, rejection, or complex medical and psychosocial challenges often remain under close care of transplant nephrologists. To add to this, community nephrologists may be uncomfortable managing transplant patients especially those with post-transplant complications or those receiving newer immunosuppressants such as belatacept. Patients can become caught in the middle, unsure which team to contact for medication refills, test follow-up, or urgent concerns. These communication gaps highlight the need for a streamlined process to guide transitions between transplant centers and referring nephrologists.
Active engagement between transplant centers and referring nephrologists is critical to sustain good long-term kidney transplant outcomes. Recognizing this need, the American Society of Transplantation (AST) convened a Controversies Conference in October 2022, bringing together a multidisciplinary coalition including transplant nephrologists, general nephrologists from both academic and private practice, and representatives from the National Kidney Foundation (NKF), Renal Physicians Association (RPA), American Society of Nephrology (ASN), American Association of Kidney Patients (AAKP), and CMS. The conference focused on identifying barriers and strategies for optimizing the transition of care for kidney transplant recipients from transplant nephrologists back to referring nephrologists.
One key takeaway from the conference was that successful transitions depend on a clearly defined partnership between transplant nephrologists and referring nephrologists. Establishing a formalized, collaborative care framework improves recipient outcomes and enhances system efficiency by reducing complications. To achieve this, it is critical that referring nephrologists understand their role in long-term recipient care delivery, including monitoring immunosuppression, screening for comorbidities, recognizing complications early, and understanding when to refer the patient back to the transplant centers for transplant-specific complications. On the other hand, transplant nephrologists should provide the referring nephrologists a thorough, standardized transplant summary at the time of transition that details immunosuppressive history, complications to date, infection risks, monitoring guidance, and specific follow-up expectations. This communication should clearly delineate which aspects of care can be managed locally, when to involve the transplant team, and how to reach them for urgent concerns. The transplant team should remain readily accessible to both the patient and their general nephrologist for transplant-specific concerns that may arise after the transition of care (Figure 1).
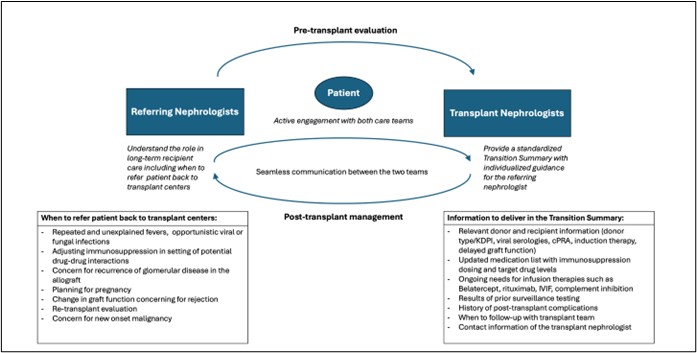
Figure 1. Outline of the collaborative relationship between transplant nephrologists and referring nephrologists. © Lee and Khairallah.
An equally important component of a successful transition in post-transplant care is patient empowerment. The transition back to the referring nephrologist should be framed as a natural and positive step within the shared-care model and a marker of a successful transplant course. Early on in their post-transplant course, patients should be educated on how to access and interpret results and understand their immunosuppressive targets. They should also be given clear instructions on when and how to contact their general nephrologist versus transplant team. Empowering patients to take an active role in their care promotes confidence and adherence as they navigate between two teams within this shared-care model.
Another major theme that emerged from the AST conference was the recognition that long-term transplant care encompasses more than immunosuppression management and serum creatinine monitoring. Recipients face increased risks of infection, cardiovascular and metabolic complications, recurrence of glomerular disease, and malignancy. Referring nephrologists are capable of integrating these domains into routine chronic kidney disease management, provided they are supported with guidance from the transplant team. Further guidance on these issues is provided in the report and provides a helpful reference for practicing nephrologists.
In summary, the conference outlines the following key strategies to improve transition of care:
Formalized transition processes |
Develop standardized, institution-wide protocols to ensure consistent patient handoff and follow-up. |
Clear roles |
Clearly delineate the responsibilities of transplant centers and referring nephrologists to avoid gaps or redundancies in care. |
Referral thresholds |
Establish guidelines for when patients should return to the transplant center, such as episodes of acute rejection, complex infectious complications, or allograft dysfunction. |
Training and education |
Incorporate transplant-related competencies into general nephrology training programs to ensure general nephrologists can confidently manage long-term transplant recipients. |
Patient-centered communication |
Ensure patients and their support networks understand the shared-care model and receive information about management expectations. |
The conference also acknowledged several current limitations to this shared-care model. General nephrologists, often driven by workforce shortages, competing clinical demands, and variability in confidence and capacity to care for transplant recipients, may not be comfortable managing transplant recipients long-term. Therefore, adapting nephrology fellowship training to the growing numbers of transplant recipients is key. Future nephrologists should be better prepared for the complexities of transplant recipient management. Reimbursement barriers were another focus, as current CMS financial models primarily incentivize transplantation rather than post-transplant care. Additionally, the optimal timing of care transition lacks consensus, with some centers adopting rigid protocols while others using individualized approaches based on clinical stability and local care availability. Patient reluctance to transition is another barrier. Finally, limited re-engagement of primary care providers (PCPs) was identified as a persistent challenge, and involving PCPs in the transition through providing education and close coordination from early post-transplant days can streamline the shared care process.
The AST Controversies Conference highlights that caring for kidney transplant recipients is multidisciplinary. One nephrologist cannot manage all aspects of their complex, lifelong care. The success of kidney transplantation depends on shared responsibility between the transplant nephrologist, transplant center and referring nephrologist, sustained by clear communication, standardized protocols, and patient-centered education. By promoting and continuously refining shared-care models for kidney transplant recipients, the nephrology community can rise to meet the demands of a growing transplant population while sustaining excellence in long-term outcomes.
-Post prepared by Deborah Lee and Pascale Khairallah
To view Anand et al [Subscription required], please visit AJKD.org:
Title: Transition of Care of Kidney Recipients from Transplant Centers to Referring Nephrologists: Report From the American Society of Transplantation Controversies Conference
Authors: Prince Mohan Anand, Neeraj Singh, Gaurav Gupta, Mona Doshi, Bekir Tanriover, Deborah Adey, Krista L. Lentine, Silke Niederhaus, Ronald F. Parsons, Alexander Wiseman, Matthew Cooper, Gary Singer, Darshana Dadhania, Roy D. Bloom
DOI: 10.1053/j.ajkd.2025.06.016


Leave a Reply