KDIGO CKD-MBD Updated Guideline: The More We Know, The Less We Know

The KDIGO Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD) Guideline Update was released last month. The team at KDIGO, as usual, did a great job presenting the update for people with differing needs and goals. The guideline update comes in three serving sizes:
- The complete guideline, with a lengthy editorial justifying the guideline including a summary of the evidence and comprehensive references. If you are starting fellowship and want to know not just what we do but why we do it, go to this version and read it from front to back (59 pages). It will make you smarter.
- There is a Summary of the guideline. This is just the bare bones of what the guideline says, with the evidence grades for each guideline. If you trust KDIGO and just want to know what they say, then this two-page sheet will be just right for you.
- The last component of the trifecta is the Executive Summary (11 pages). This document provides the tick-tock details of how the committee approached each guideline and what they were thinking when the changes were made. If you want to get a feel for how and why the changes were made and get a hint of the acrimony behind the text, this is the document for you.
Looking at the new guideline, there are 15 changes from 2009. Some of these changes are due to improved knowledge from well-done prospective and interventional trials to replace the cross-sectional and observational data that underpinned much of the original guideline. This is most clearly seen in the areas of osteoporosis where new data in CKD patients have shown bone mineral density (BMD) tests to be validated for assessing fracture risk in CKD patients. Additionally, physicians have gained experience with anti-resorptive agents in CKD, so the guideline no longer recommends a bone biopsy prior to prescribing these agents. (See guideline recommendations 3.2.1, 3.2.2, 4.3.3, 5.5, 5.6).
But other recommendations have changed less because of new data and more due to changing expectations and increasing humility with regards to guideline recommendations in general. Take a look at what the Executive Summary had to say on the recommendations for phosphorus in CKD:
The Work Group drew several conclusions:
- The association between serum phosphate and clinical outcome is not monotonic;
- Evidence is lacking to demonstrate the efficacy of phosphate binders for lowering serum phosphate in patients with CKD G3a to G4;
- The safety of phosphate binders in this population is unproven; and
- There is an absence of data showing that dietary phosphate restriction improves clinical outcomes.
Consequently, the Work Group has abandoned the previous suggestion to maintain phosphate in the normal range, instead suggesting that treatment be focused on patients with hyperphosphatemia.
Looking at the 4 conclusions for the change in the guideline, none of them are dependent on new data. The data that is lacking in 2017 was also lacking in 2009. The data didn’t change, but the interpretation did. KDIGO was no longer willing to take the leap of faith. Granted, the actual change in the guideline was pretty subtle, but I am encouraged by this and hope for more adherence to strict evidence standards, patient-oriented outcomes, and prospective, randomized, controlled, 1A-evidence.
Looking over the guideline in total, one can’t help but be a bit depressed. A grade heatmap below (note some recommendations have more than one grade):
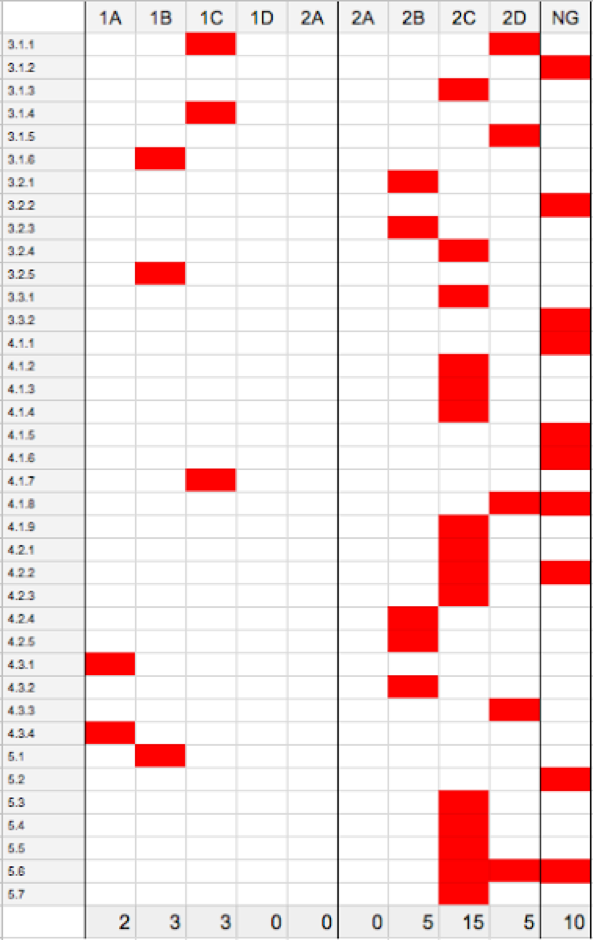
There are 38 separate guideline recommendations representing 43 scores; of these, 10 are not graded. Looking at the 33 evidence grades, 23 are C and D level, meaning the quality of the evidence is either low or very low. Only 2 of 43 recommendations are A-level evidence, ie a high grade of evidence with a large degree of certainty that the true effect is close to the estimate.
KDIGO provides research recommendations for each guideline, but despite nearly a decade between the original guideline and this update, only a single guideline improved its evidence score (4.1.4: recommending a dialysate calcium bath of 1.25 to 1.5 mmol/L improved from 2D to 2C).
Nephrology has long bemoaned the lack of prospective trials. Poor evidence and lack of progress in improving it show that the way we have been handling patient-oriented research may be failing both doctors and patients. It is time for new ideas to break the evidence stalemate.
– Post prepared by Joel Topf, AJKD Social Media Advisory Board member. Follow him @kidney_boy.

I fully do agree that 2017 kdigo CKD MBD guidelines are not much different from that of 2009. I think we as Nephrology committee should think out of the box to find a reasonable solution for CKD related problems in the reality rather than publishing unnecessarily many useless publications.