Statin Use in Chronic Kidney Disease: An Interview
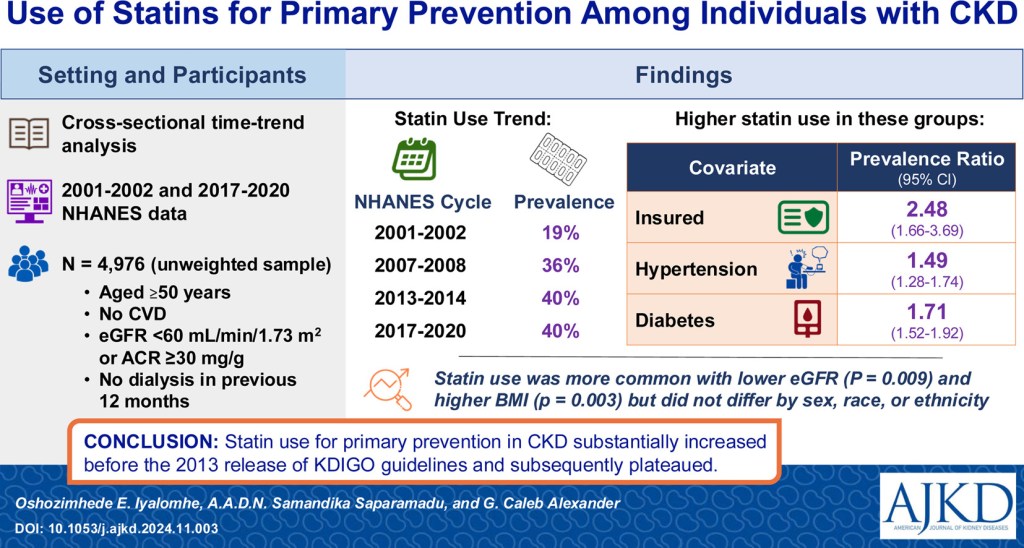
Chronic kidney disease (CKD) populations face an elevated risk of cardiovascular disease (CVD), yet many remain undertreated with statins for primary prevention of CVD despite meeting eligibility criteria. In an investigation published in AJKD, Iyalomhe and colleagues examined trends in statin use for primary prevention among individuals with CKD before and after the release of the 2013 Kidney Disease: Improving Global Outcomes (KDIGO) guideline recommending statin use for lipid management. Recently, AJKDBlog Interviews Editor Timothy Yau (@Maximal_Change) chatted with Dr. Iyalomhe about statin use in the CKD population.
Oshozimhede E. Iyalomhe, MD, MPH is a PhD scholar in epidemiology at the University of Maryland School of Medicine, leveraging his experiences as a physician in population health research and drug therapy optimization for underserved populations.
AJKD Blog: Before we jump into the actual article, can you give us a quick background on some of the major trials looking at statin use in CKD? I was a fellow when negative trials demonstrating cardiovascular benefit of statins in patients on dialysis (AURORA, 4-D), but the SHARP trial gave us a glimmer of hope for some benefit in CKD. Can you familiarize our readers with a synopsis of some of the major trials (some of this may segue into the next question, as well)?
Dr. Iyalomhe: Three landmark clinical trials have shaped our understanding of statin therapy in CKD.
The 4-D trial, published in 2005, was one of the first to test statins in CKD. It included over 1,200 individuals with diabetes on hemodialysis, who were randomly assigned to receive daily atorvastatin or placebo. Atorvastatin did not statistically significantly reduce the composite outcome of heart attack, stroke, or cardiovascular death after nearly four years of follow-up. This was despite an earlier reduction in low-density lipoprotein (LDL) cholesterol by 40% compared to 1% in the placebo group. These findings were unexpected, given the established cardiovascular benefits of statins in the general population.
A few years later, the AURORA trial tested rosuvastatin in a much larger group of dialysis patients—more than twice the size of the 4-D trial. Again, LDL cholesterol dropped by 40%, but there was no statistically significant reduction in cardiovascular events. These disappointing results raised concerns that statins might not work the same way in people with advanced kidney disease, possibly due to factors like vascular stiffness, calcification, and overactivity of the sympathetic nervous system.
However, in 2011, the SHARP trial provided more encouraging findings. As the largest study of its kind, enrolling more than three times the number of participants in AURORA, it included both dialysis and non-dialysis CKD patients. SHARP demonstrated that simvastatin plus ezetimibe reduced the risk of heart attacks, strokes, and other major cardiovascular events by 17%. Importantly, this benefit was seen regardless of baseline cholesterol levels.
These findings had a major impact on clinical guidelines. The disappointing results from 4-D and AURORA led to recommendations against starting statins in dialysis populations. However, the positive findings from SHARP showed clear benefits for people with CKD who were not yet on dialysis, supporting statin use in this broader population.
AJKD Blog: One of the pivotal moments in this field came in the 2013 guidelines recommending statin use for adults with CKD. Can you give us some specifics on why this recommendation changed at this time?
Dr. Iyalomhe: The 2013 guideline update emerged from almost a decade of research that had built strong evidence on the benefits of statins, both in the general population and in people with CKD. The SHARP trial was the catalyst, showing that statins could reduce the risk of heart attacks and strokes in CKD patients—even beyond just lowering cholesterol. Before this, we knew statins worked well for heart disease prevention in people without kidney disease. But because CKD affects the cardiovascular system in unique ways, it wasn’t clear whether statins would have the same benefits. This uncertainty created a need for clear, evidence-based guidelines.
In response, KDIGO (Kidney Disease: Improving Global Outcomes) convened a workgroup to focus on cholesterol management in CKD. Their goal wasn’t just to summarize research but to provide practical recommendations that clinicians could use in everyday patient care. The result was the 2013 guideline update, which strongly supported statin use in adults with CKD to help reduce cardiovascular risk.
AJKD Blog: Now to this publication, what were your goals as the investigators when designing this trial, and what did you expect to find?
Dr. Iyalomhe: Our main objective was to determine whether the 2013 guideline recommendations contributed to an increase in statin use among adults with CKD who were eligible for treatment. We also wanted to understand what factors influenced prescribing patterns.
We expected to see a rise in statin use after the guideline update. To examine this, we analyzed data from the National Health and Nutrition Examination Survey (NHANES) to track changes in statin prescriptions over time. Our study was driven by previous research and reports from clinical practice and social media, which suggested that, despite strong evidence and clear guidelines, many individuals with CKD were still not receiving statins as recommended.
AJKD Blog: You utilized the NHANES database, can you tell us about this cohort, what individuals you identified, and what variables you included in your analysis? Ultimately what was the primary outcome you were looking at?
Dr. Iyalomhe: We chose NHANES because it provides a comprehensive snapshot of health trends across the U.S. This large, federally-run survey, typically conducted in two-year cycles by the National Center for Health Statistics, uses a structured sampling method to ensure a nationally representative selection of the non-institutionalized U.S. population. This approach allows us to make reliable population-level estimates about health behaviors and medical treatment patterns.
For our study, we analyzed nearly two decades of NHANES data (2001–2020), focusing on individuals who met the KDIGO guideline criteria for statin therapy. Specifically, we included adults aged 50 and older with CKD who had no history of cardiovascular disease and were not on dialysis.
Our primary objective was to examine trends in statin use over time. We also explored factors influencing prescription patterns, including sociodemographic characteristics (age, race/ethnicity, gender, education, income, and insurance coverage) and clinical factors (body mass index, diabetes, hypertension, cholesterol levels, and kidney function measures). This comprehensive approach helped us understand who was receiving statins and what factors influenced their use in CKD patients.
AJKD Blog: With all the trials and data we discussed earlier, what trends did you notice from 2001 through 2020? Were there any other variables that stuck out or surprised you in the analysis?

Trends in statin use for primary prevention among chronic kidney disease population Figure 2 from Iyalomhe et al, © National Kidney Foundation.
Dr. Iyalomhe: Our analysis revealed a sharp increase in statin use in the early years, nearly doubling from 19% in 2001–2002 to 36% by 2007–2008. However, after this initial rise, statin use plateaued. By 2013–2014, approximately 40% of eligible individuals were on statins, and this rate remained steady through 2017–2020. This early surge likely reflects the emphasis on high-intensity lipid-lowering therapies to achieve lower LDL cholesterol levels.
One unexpected finding was the lack of race/ethnic disparities in statin use, which differs from previous studies in less representative populations. This suggests a need for better representation of race/ethnic minorities in research and equitable care across all populations. As expected, individuals with health insurance were more likely to receive statins, highlighting access to care as a key determinant of treatment. Additionally, those with hypertension or diabetes were more likely to be prescribed statins compared to individuals with CKD alone hinting at its underuse in the presence of CKD alone.
AJKD Blog: In your discussion, you mention that although statin use doubled between 2001-2002 to 2007-2008, still only one in three individuals received the drug for primary prevention. Is this incidence surprising, and what are some reasons for this lower than expected number?
Dr. Iyalomhe: Yes, these findings are unexpected, given the well-documented cardiovascular risk in CKD. The gap between guideline recommendations and real-world practice is evident, as adults 50 years and older with CKD consistently have a 10-year risk of coronary death or non-fatal myocardial infarction exceeding 10%, regardless of other comorbidities.
One factor contributing to lower-than-expected statin use in this population is the historical focus on LDL cholesterol levels rather than overall cardiovascular risk. Earlier guidelines emphasized cholesterol targets and high-intensity statin therapy, but we now understand that LDL cholesterol alone does not fully capture cardiovascular risk in CKD. This shift in perspective led KDIGO to recommend statins for all individuals with CKD aged 50 and older (not on dialysis), simplifying clinical decision-making by removing the need for complex risk calculations.
However, several real-world barriers limit the adoption of these recommendations. Clinicians face increasingly complex patient populations and must navigate a rapidly evolving landscape of medical guidelines and evidence. In practice, treating patients with multiple comorbidities often means competing priorities, making statin initiation less of an immediate focus. Additionally, patient-related factors, such as concerns about polypharmacy, medication costs, and potential side effects, play a significant role in both prescribing decisions and adherence to statin therapy—particularly in CKD, where managing multiple medications is already challenging.
AJKD Blog: Any closing thoughts, and how do you think your paper can inform current clinical practice?
Dr. Iyalomhe: A key takeaway from our research is the disconnect between evidence and clinical practice. Despite strong evidence supporting statin safety and efficacy in CKD, as well as clear guideline recommendations since 2013, we did not observe an increase in statin use even seven years later. This is concerning, given that statins provide significant cardiovascular benefits in CKD that are independent of LDL cholesterol levels.
Our findings have important implications for clinical practice. They underscore the need for implementation science strategies to effectively translate guidelines into routine care. Sustained engagement with stakeholders—including clinicians, healthcare systems, and policymakers—will be critical in addressing barriers to statin use. Perhaps more importantly, our study highlights the need for improved cardiovascular risk assessment and thoughtful consideration of statin therapy for each individual with CKD.
To view Iyalomhe et al [Subscription Required], please visit AJKD.org.
Title: Use of Statins for Primary Prevention Among Individuals With CKD in the United States: A Cross-Sectional, Time-Trend Analysis
Authors: Oshozimhede E. Iyalomhe, Amarasinghe Arachchige Don Nalin Samandika Saparamadu,∙ and G. Caleb Alexander
DOI: 10.1053/j.ajkd.2024.11.003

Leave a Reply