ESRD Patients Living Longer, But Could We Have Done Better?
“On a long enough timeline, the survival rate for everyone drops to zero” –Edward Norton, Fight Club
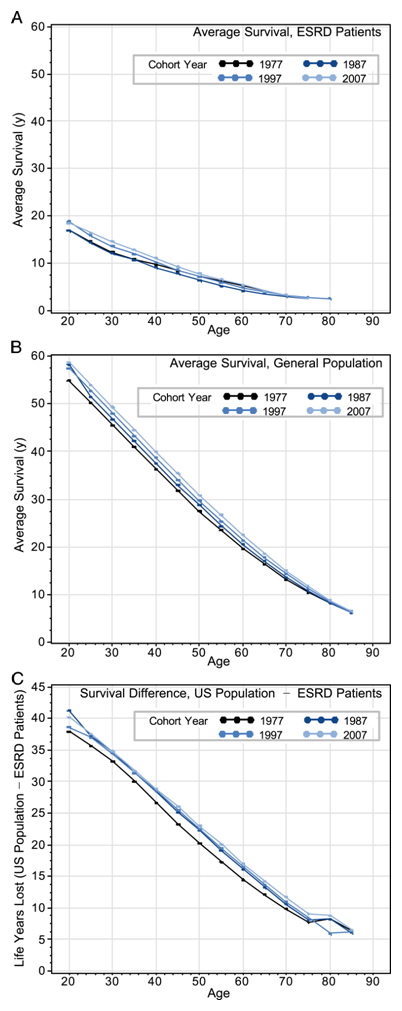
In a recent article in AJKD, van Walraven et al highlight the trends in ESRD patient survival over the last three decades. Their study was based on an analysis of US Renal Data System records of ESRD patients who received renal replacement therapy (dialysis or transplantation) in the years 1977, 1987, 1997, and 2007. First, the good news: age-specific survival in ESRD patients improved through these years, even though patients tended to be older and sicker with more comorbidities and mortality risks. This is heartening, and the reasons for the improvement in this all-cause mortality have been variously attributed to an increased proportion of patients with ESRD receiving a transplant (which we know is associated with improved survival), better management of diabetes mellitus and its complications (since the proportion of diabetes-related ESRD went up from 10% in 1977 to about 40% in 2007). This is also consistent with prior data showing a 16% decrease in mortality in established ESRD patients beyond the first year of dialysis, between 1985 and 2009.
A further analysis, however, tempers the good news with some sobering realizations. The authors also compared the differences in age-specific relative life expectancy between an average person and an ESRD patient across 1977 to 2007. This unfortunately has actually worsened over these thirty years. Thus, even though an ESRD patient initiating renal replacement today can expect to live longer in absolute terms than someone who started similar treatment in 1977, they now have “more to lose” in terms of lifespan, compared to the average person!
There are multiple reasons for this widening survival gap between the general population and the ESRD population. Clearly, the improvement in ESRD survival has been held back by factors such as dialysis catheter use, and perhaps a misplaced priority on surrogate end points used to prescribe dialysis adequacy (Kt/V?). Another contributing factor is that the average ESRD patient today is sicker, with the author-defined “high risk” patient prevalence increasing from 36.8% to 50.7%. However, a discussion about relative survival is incomplete without understanding why US life expectancy has shown a bigger improvement in the corresponding period. While the ESRD population continues to age and grow sicker, the general population has reaped the benefits of strides made in the treatment of cardiovascular disease, cancer, etc. One could then argue that relative survival for ESRD patients is worse now simply because the general population is doing so much better. Our ESRD patients, in spite of making progress, still lag behind.
So why haven’t better treatments for cardiovascular disease touched the lives of our kidney failure patients? Are ESRD patients just different, with unique pathophysiology of cardiovascular disease from a non-ESRD patient? Calcium deposition plays a central role, and even though garden variety atherosclerosis could still be important, statins have not been shown to be helpful (as per its recently released guidelines, KDIGO does not recommend initiating statins in dialysis-dependent CKD).
The study has its limitations. The authors acknowledge that their analysis did not control for GFR at initiation of renal replacement, and for comorbid conditions. These are important points to note. We understand that given the recent evidence, there is now a trend towards starting dialysis at lower GFRs than before. This could imply that patients in the earlier cohorts were less sick, thus creating a selection bias of superior relative survival.
We also need to appreciate the profound impact that comorbidities have on ESRD patient survival. In older ESRD patients with a high comorbidity burden, there seems to be no significant survival difference between patients who are treated with dialysis as opposed to conservative management! In such a situation, dialysis might not be expected to create significant survival improvements over the years since the patients have also got progressively sicker. Finally, dialysis vintage which is associated with an increase in the relative risk of death is much longer in the 2007 cohort (4.2 years), than in the 1977 cohort (1.7 years).
All said and done, this study provides some interesting insights in to how the survival landscape has changed over three decades for our ESRD patients. We seem to have made some progress, but not quite as much as we would have liked.
Veeraish “VC” Chauhan, MD
eAJKD Contributor
To view the article abstract or full-text (subscription required), please visit AJKD.org.

Leave a Reply