#NephMadness 2017: Disparities in Nephrology Region

Copyright: lassedesignen / Shutterstock.com
Submit your picks! | NephMadness 2017 | #NephMadness or #DisparitiesRegion
Selection Committee Member for the Disparities Region:
L. Ebony Boulware
Dr. Boulware, MD, MPH, is Professor of Medicine, Chief of the Division of General Internal Medicine in the Department of Medicine, Vice Dean for Translational Science, and Associate Vice Chancellor for Research in the School of Medicine at Duke University. She has spent the majority of her scholarly career investigating mechanisms to improve the quality and equity of care and health outcomes of patients and populations with chronic diseases such as CKD and hypertension.
Competitors for the Disparities Region
Genes in ESKD Disparity vs Society in ESKD Disparity
Patient Factors in Transplant Disparity vs System Factors in Transplant Disparity
Disparities in End Stage Kidney Disease (ESKD)
ESKD represents an enormous public health problem nationwide with huge economic burden. According to the US Renal Data System (USRDS) Annual Data Report, more than 468,000 Americans are on dialysis and of these, more than 89,000 people with ESKD die every year. The one-year mortality rate of dialysis patients is 20-25% and only about 50% of dialysis patients are alive 3 years after starting dialysis. Striking racial and ethnic differences are present in the incidence, prevalence and long-term outcomes in dialysis patients.
- Even though African Americans represent only 13% of the overall U.S. population, they constitute more than 35% of all patients that receive dialysis.
- The age-adjusted incidence of ESKD in African Americans is 4 times higher than whites.
- For Native Americans and Hispanics, risk of ESKD is 1.5 times higher.
- Asian and African Americans had the highest likelihood of successful AV fistula use at hemodialysis initiation and females are less likely to have an AV fistula placed as compared to males.
Interestingly, the risk of death is 45% lower in African Americans than whites undergoing chronic hemodialysis, and age seems to be an effect modifier (i.e. younger African Americans patients have poorer survival and older African Americans have better survival than whites). Apart from racial differences, huge gender disparities also exist in ESKD patients.
Fewer women than men receive dialysis treatment in the US (43% vs. 57%) despite a higher prevalence of CKD in women as compared to men in the National Health and Nutrition Examination Survey (15% vs. 12%). Surprisingly, the survival advantage that women have over men in general population is markedly diminished in dialysis patients. These disparities raise the possibility that differential access to health care and probably faster progression to ESKD, may be a cause for concern in minority groups. Is this all on the basis of socio-economic factors, or do genes matter? The first round of NephMadness features two prominent factors both with complex interplay. The first factor is the role of genetics in the enhanced risk of ESKD in African Americans, an issue that was put front and center with the discovery of the APOL1 risk alleles (2015’s winning team). This is contrasted with the societal factors, which also exert powerful effects on kidney disease progression. Is nature or nurture to blame?

Vol 2 Figure 1.5 from USRDS 2016 ADR, © USRDS. Rate of incident ESKD adjusted for age and sex. The standard population was the U.S. population in 2011.
Genes in ESKD Disparity

Copyright: Arthimedesa / Shutterstock.com
One of the biggest advances in nephrology was the landmark paper reported in Science that highlighted the importance of genetics in addressing disparities in ESKD. Despite a similar prevalence in earlier stages of CKD, African Americans have an increased risk of ESKD as compared to whites, which suggests that kidney function declines more rapidly after the onset of CKD in African American patients. Genes may explain the racial disparities in the rates of ESKD. Apolipoprotein L1 (APOL1) variant is one of the first major discoveries of genetic variants that substantially increases the risk of ESKD in African Americans. Two separate disease-causing polymorphisms located in the last exon of APOL1 gene (the G1 and G2 risk alleles), which follow an autosomal recessive pattern of inheritance, confer a 10-fold higher risk of ESKD due to focal glomerulosclerosis and 7-fold higher risk of ESKD caused by hypertension. Regardless of the cause, African Americans with two APOL1 high-risk variants have a higher risk of CKD progression and faster decline of glomerular filtration rate as shown in the Chronic Renal Insufficiency Cohort (CRIC) study. In the African American Study of Kidney Disease and Hypertension (AASK) study, which enrolled African American patients with CKD attributed to hypertension, about 60% of patients in the APOL1 high-risk group had progression to the composite renal outcome defined as a doubling of the serum creatinine level or incident ESKD. APOL1 mutations are also associated with an earlier onset of kidney disease and African Americans carrying two copies of the G1 risk allele are significantly younger at the time of dialysis initiation than those without APOL1 risk alleles. Genetic differences are an important piece of the disparities-ESKD puzzle; and although these racial differences could have socioeconomic components such as access to care, the genomic part of this puzzle cannot be ignored. Genomic information gives us many opportunities to improve clinical outcomes in patients with kidney disease including the use of APOL1 genetic screening for risk stratification and preventative interventions with the goal of identifying and intervening much earlier than the present standard of practice. Currently, the adoption of genomics by providers during routine clinical care of patients with ESKD is limited. Efforts like those by the Implementing GeNomics In pracTicE (IGNITE) group of the National Human Genome Research Institute aim to improve genomic literacy of physicians and implement clinical decision support systems through identification of educational needs and sharing of educational approaches.
Society in ESKD Disparity

Copyright: Laurin+Rinder / Shutterstock.com
African Americans, Hispanics, Native Americans, and Asian Americans all have elevated risks of developing ESKD. The reasons for this are not entirely clear and cannot be explained entirely by physiologic and pathologic factors. Even rockstar genes like APOL1 result in abstracts using phrases like
- “APOL1 risk variants weakly predict mild forms of kidney disease,”
- “however, these variants alone are insufficient to produce disease”
- “The high variability in eGFR decline among blacks with and without the APOL1 high-risk genotype suggests that population-based screening is not yet justified.”
Social and economic factors like median income, health insurance, geography and access to health care are important determinants of outcomes in patients with ESKD. Socioeconomic status (SES) can be a critical factor in some etiologies of ESKD. Ward looked at socioeconomic status by zip code and correlated it to the rates of ESKD from diabetes and autosomal dominant polycystic kidney disease (ADPKD). He found a strong inverse correlation for diabetes (lower SES associated with higher rates of ESKD) and no relationship with ADPKD. A more general look at the association of income and CKD was done by Vart, et al. They found an odds ratio (OR) of 2.74 for income in the lowest quintile compared to the highest. Similarly there was a relationship between education and CKD, with an OR of 1.78 for the lowest quintile compared to the highest.
These disparities can take various and unexpected form. In a 2015 paper, Suarez et al showed that about 10% of NHANES participants lived in food deserts (more than 1 mile from a grocery store in urban areas, or more than 10 miles if in rural areas). People living in food deserts were more likely to be African Americans or Hispanics. Residents of food deserts also had higher systolic blood pressure. There was not an association with CKD, however, low income was associated with CKD. Living in a food desert was associated with a notably poorer diet including a higher daily acid load and lower potassium intake.
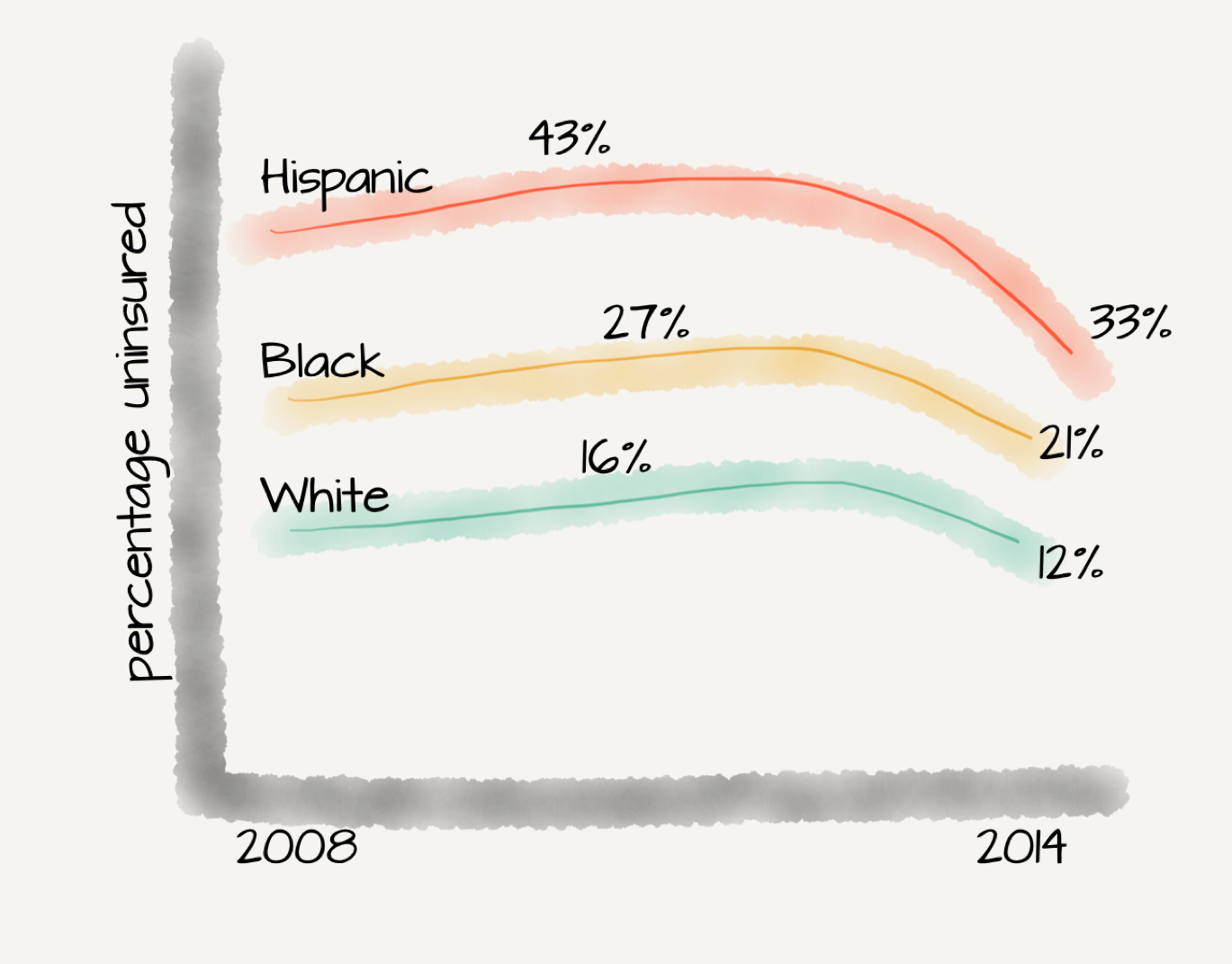
The first few years of the Affordable Care Act has seen a narrowing in the racial difference in uninsurance rates. The narrowing gap is being led by states that expanded Medicaid.
Further complicating the analysis is that once African Americans progress to dialysis they have a distinct survival advantage that has been difficult to understand. Some of it is explained by case-mix, but this phenomenon remains largely unexplained. African American dialysis patients living in highly segregated neighborhoods do worse than African Americans living in integrated neighborhoods. Segregation has not been shown to be related to survival among Whites. O’Hare et al showed that the incidence of ESKD becomes progressively higher in regions with greater intensity of health care among all older whites aged 65 years or more, but interestingly, this trend is limited to those African Americans of advanced age (men aged 80 years or more, women aged 85 years or more). Living in a neighborhood with a lot of income inequality, however, decreased survival for whites but did not affect African American survival on dialysis.
Pre-dialysis health care is important in patients with kidney disease since patients under nephrologist care are more likely to receive AVF and have reduced first-year dialysis mortality. Socioeconomic disparities result in variations in pre-dialysis care with poorer patients and patients of African American and Hispanic ethnicity having lower likelihood of pre-ESRD nephrology care. In a study by McClellan et al, women and older patients were more likely to receive at least six months of pre-dialysis care from a nephrologist.
The existence of health disparities in ESKD patients therefore provides an unusually powerful and unrecognized opportunity for understanding how biological, sociocultural and health care system factors may affect clinical outcomes. Minority populations are disproportionately affected by ESKD, and given interdependency of race, ethnicity and socioeconomic factors on adverse clinical outcomes, it becomes important to focus on these minority groups to improve long-term outcomes. It is incumbent on nephrologists to direct interventions at highly segregated African American neighborhoods to favorably improve patient outcomes.
Disparities in Transplantation
Kidney transplant (the inaugural #NephMadness champion) offers the best hope to patients with ESKD since it improves survival, offers better quality of life, and is more cost effective than dialysis. It has already been demonstrated that African Americans, Hispanics and Native Americans are over-represented in the ESKD population in the US, as is true of African American and Asian populations in the UK. Compounding this issue is that, as compared to whites, African Americans with ESKD are reported to have longer waiting times, reduced rates of living donor transplantation, shorter graft survival and a more rapid progression to chronic allograft nephropathy.
- Once on the wait-list, African Americans have to wait 40% longer than whites.
- African Americans have a lower chance of receiving a kidney transplant from living donors (23% versus 43%) as compared to whites.
- African Americans are less likely to complete evaluation as compared to whites (26% versus 52%).
In a large study from the UNOS Scientific Transplant Registry, Isaacs et al concluded that African American patients were 1.7 times more likely than white patients to experience kidney graft failure during the 9-year follow up. The mean time to chronic allograft nephropathy has also been demonstrated to be shorter in African American recipients than in white patients (18 vs. 37 months). The presence of health disparities in transplant outcomes constitutes a public health problem and could be attributed to the variety of patient and system related factors. Understanding how these factors affect specific steps in the transplant process may help identify interventions to reduce the sociodemographic differences that currently exist in kidney transplantation rates.
Patient Factors in Transplant Disparity

Copyrigaht: Monkey+Business+Images / Shutterstock.com
How do “patient” factors figure into the inferior kidney transplant outcomes and lower transplantation rates in patients with ESKD? It is important to consider several patient related factors in this scenario like innate biological and medical variables, lack of knowledge about transplantation compounded by poor health literacy, and legitimate concerns about surgery, adverse effects of medication, and health care costs.
Attitudes and behavior often influence the likelihood that a patient will appear on a transplant wait list. Compared to whites, African American patients with ESKD are 3-5% less likely to want a transplant, and tend to express uncertainty about the benefits of having a transplant. Unsurprisingly, they are also less than half as likely to complete the pretransplant workup process successfully. Women and poor individuals are also about 20% less likely to complete pretransplant workup. Why is this? Not only do they start off with a lower knowledge base, but they are also less likely to talk to their family and friends, less willing to allow a living donor to volunteer, and less likely to get on the deceased donor waitlist. Patient interest, perception, willingness, subconscious bias and knowledge have an important role to play in the disparities that currently exist in access to renal transplantation. Interestingly, controlling for initial patient knowledge completely attenuated the disparities in receipt of kidney transplant. Thus, lack of understanding about kidney transplantation could be viewed as an opportunity rather than a threat, and early patient education (particularly in settings like community nephrologists’ offices and dialysis centers) might be a key corrective step. The modality of education also matters – while dialysis care providers communicate to their patients the advantages of having a transplant, poor health literacy in CKD tracks alongside poverty and minority status and is associated with lower rates of transplant listing. However, most educational material in CKD has limited readability – this systematic review suggests that only 5% are at the recommended grade 5 level. Hence specific techniques, such as face-to-face sessions, interactive teaching, involvement of family members, goal setting and using teach-back methods are some effective ways of getting the message across.
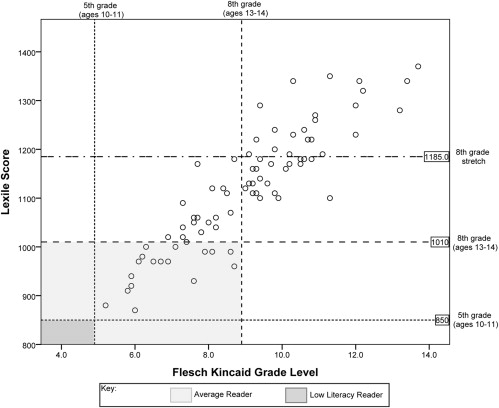
Figure 2 from Morony et al, AJKD, © National Kidney Foundation.
Correlation between Lexile and Flesch-Kincaid results. Dotted horizontal lines indicate the 75th percentile of 5th grade (850L) and 8th grade (1,010L) Lexile text scores. Upper horizontal line is the 75th percentile of “stretch” (Common Core State Standards) 8th grade text scores. Vertical lines indicate upper limit of Flesch-Kincaid scores for grades 5 (5.9) and 8 (8.9). Light shaded area represents patient materials that could be read by the “average” patient. Dark shaded area represents materials that could be read by a low-literacy patient.
Lastly, the issue of financial coverage around and after kidney transplantation contributes to the unwillingness to undergo waitlisting. Worries about surgical cost are accentuated by lack of social support among those with lower socioeconomic status. Lack of post-transplantation immunosuppression medication coverage, still an ongoing problem in some parts of the world, is associated with nonadherence and poor transplant outcomes.
Donation rates are lower among minorities – despite about 10% being on waitlist, only 3% of minorities are registered for organ donation. Not surprisingly, live organ donation rates are also lower, stemming from a variety of causes. Donors face financial burden (e.g days away from work), which could be potentially be addressed with legislation. Even use of social media (eg Facebook) for solicitation of donors relies on having a large enough social network (which closely tracks with socioeconomic status), thus magnifying the existing inequities.
System Factors in Transplant Disparity

Copyrigaht: Monkey+Business+Images / Shutterstock.com
System related factors that may contribute to the existing disparities in access to transplantation in patients with ESKD include variable insurance coverage, income, physician perception, geographical location, and health policies. Whites and patients with commercial insurance are usually evaluated within 1 year of referral, in contrast with late evaluations, which occur mostly in African Americans, people residing in a lower income countries, and those with noncommercial insurance. Provider behavior also significantly impacts lower listing rates of African Americans, women, and older patients. Inappropriate exclusions occur among relatively healthy African Americans, while inappropriate classifications of candidacy occur among sicker Caucasians. African American patients are less likely than whites to be rated as appropriate candidates for transplantation (9% vs. 21%) and are more likely to undergo incomplete evaluations (47% vs. 39%). Among patients considered to be appropriate candidates for transplantation, African Americans are less likely than whites to be referred for evaluation (90 % vs. 98%), less likely to be placed on a waiting list (71% vs. 87%) and therefore less likely to undergo transplantation (17% vs. 52%). Disparities in transplant outcomes also occur by geography and graft survival is lower in patients living in the poorest areas. Patients in rural areas have a lower rate of wait-listing and transplants, while graft outcomes are comparable to urban population. Worldwide, health policies on financing immunosuppression also contribute to disparities in graft survival. Woodward demonstrated the disproportionately beneficial impact on low income groups of extending Medicare’s coverage from 1 to 3 years in the United States, and another study showed that immunosuppression coverage throughout life improves graft survival in the fourth year post-transplant.
Racial differences in access to renal transplantation are pervasive and interventions should focus on reducing the existing disparities. Efforts to allocate kidneys equitably must address each step of the transplant process. The new kidney allocation system, which gives weight to the total time patient has been on dialysis, has reduced racial disparities of transplantation in minorities with increases in the deceased donor renal transplant rate in African Americans.

Adapted fm Figure 2 from Hart et al, AJT, © American Society of Transplantation and the American Society of Transplant Surgeons. Distribution of kidney transplants by race. Kidney-alone transplant recipients, January 1, 2013 to December 31, 2015. KAS was implemented December 4, 2014.
A culturally sensitive approach using a comprehensive transplant program should be adopted. Providing holistic care that considers patients’ cultural beliefs and values through a culturally competent transplant program has been found to be associated with a reduction in disparities among Hispanics in living donor kidney transplantation. Nephrologists should focus on providing more systematic education about transplantation, offering greater encouragement to undergo evaluation for transplantation, and informing physicians about racial differences in referral rates. By making renal transplantation available to all clinically appropriate candidates who desire it, such efforts would foster greater effectiveness and racial equity in the receipt of this valuable treatment.
– Post written and edited by Silvi Shah (@silvishah) and Swapnil Hiremath (@hswapnil).



A very nice and informative article in a simple style
This is such a great section as it pits science(genes) versus society and patient versus the system. Granted this is very US centric in parts but other countries also have similar disparities (and perhaps additional ones too). As someone whose first significant grant was on targeting social needs in CKD I am hoping one of these areas makes it all the way.
Thanks Damian. We appreciate your support and should have covered this topic in a more world centric way.