Non-Vaccination for Influenza Among Patients With CKD: An Interview
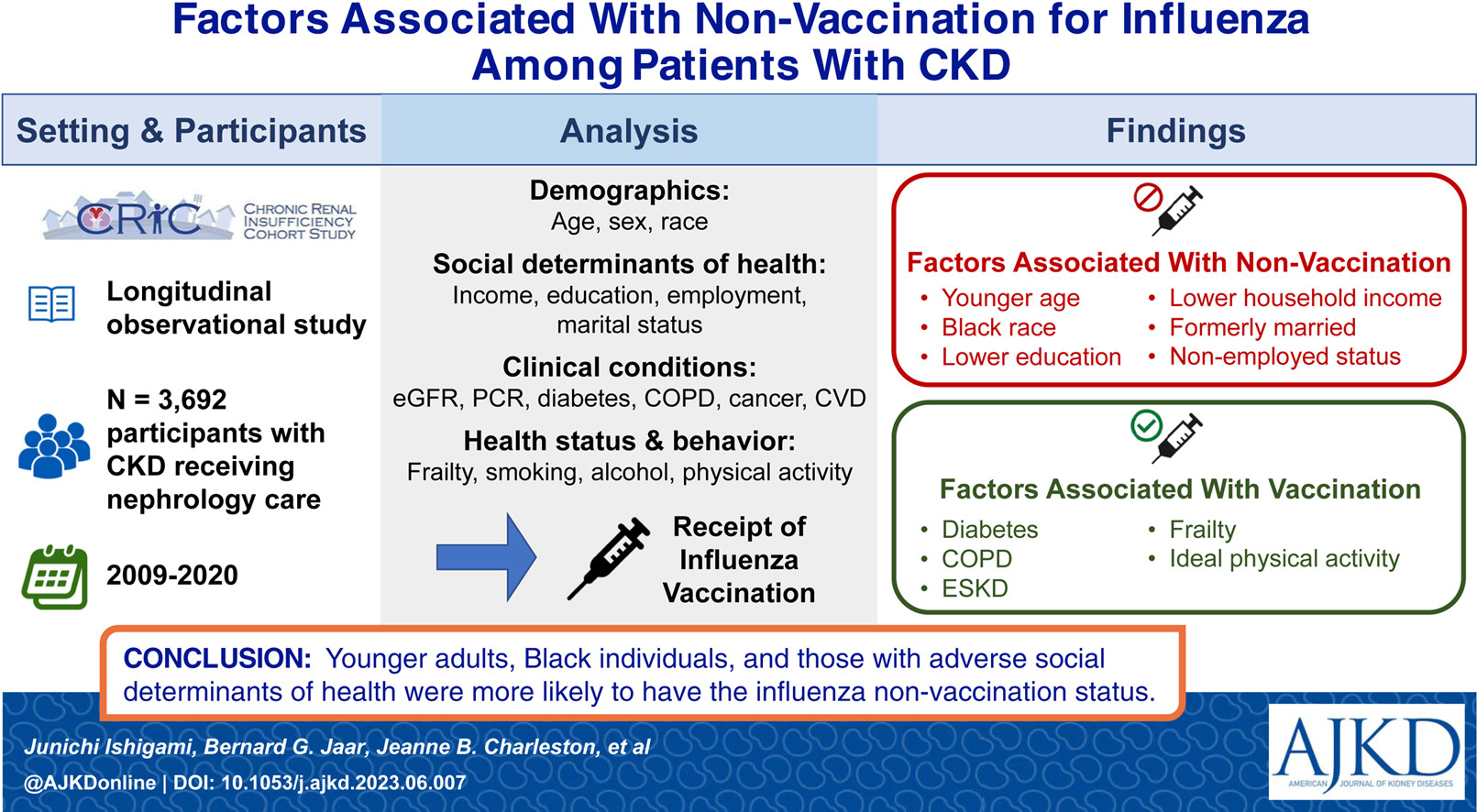
AJKDBlog Interviews Editor Timothy Yau (@Maximal_Change) had a conversation with Junichi Ishigami (@JunichiIshigami) about his recently published AJKD Orginal Investigation identifying risk factors for not receiving an influenza vaccine among patients with chronic kidney disease (CKD).
Dr. Junichi Ishigami is a clinical scientist at Johns Hopkins Bloomberg School of Public Health. His research focuses on implementation science to promote vaccinations for people with chronic kidney disease.
AJKDBlog: Thanks for highlighting this topic and asking these questions about vaccination in CKD patients in this paper. This study looked at the Chronic Renal Insufficiency Cohort (CRIC); can we start by explaining to our readers what this cohort is, and why you chose it for this study?
Dr Ishigami: Of course. The CRIC Study, supported by the National Institute of Diabetes and Digestive and Kidney Diseases, enrolled 3939 individuals with different stages of CKD from 2003 to 2008. Starting in 2008, the study regularly gathered information on the receipt of influenza vaccination among participants who were under nephrology care. Additionally, the CRIC Study compiled a range of information, including demographics, social factors affecting health, medical conditions, and behaviors related to health. With this rich pool of data, we aimed to thoroughly investigate factors associated with not receiving an influenza vaccine.
AJKDBlog: Before diving into the data, can you tell us if interventions like the flu vaccine are particularly beneficial in patients with kidney disease?
Dr Ishigami: Yes, influenza vaccination is especially important for people with CKD. Individuals with CKD have an immunocompromised condition and are at a higher risk of infection compared to those without CKD. Vaccination against influenza is a fundamental strategy to reduce the risk of getting influenza and its associated complications. Therefore, achieving a high uptake of influenza vaccination in this population is a significant public health priority. The Kidney Disease Improving Global Outcomes clinical guideline states that all CKD patients should receive immunization with the influenza vaccine as a Grade 1A recommendation.
AJKDBlog: You assessed vaccine uptake based on a questionnaire to patients during annual clinic visits. How did you differentiate between patients that may have received the flu vaccine in one year, but not in the next?
Dr Ishigami: Receipt of influenza vaccine was ascertained based on the following question, “Did you have a flu vaccine since your last CRIC visit?” This question was asked repeatedly during annual clinic visits. Consequently, each participant had the opportunity to respond to this question multiple times, and their answers might indicate receiving the influenza vaccine in certain years but not in others.
AJKDBlog: Before we get into the individual factors, what did you find globally in the CRIC participants with regards to vaccine uptake? How does this compare to studies looking at more general populations without kidney disease?
Dr Ishigami: The overall influenza vaccine uptake was 72% in the study. In the general population, the Centers for Disease Control and Prevalence estimated that influenza vaccination coverage was 46.9% in adults ≥18 years, and 69.7% in ≥65 years in the 2022-2023 influenza season. Another study for US adults with CKD using data from the National Health Interview Survey reported that the uptakes of influenza vaccine were 60-65%. These rates were higher than the general population’s but slightly lower than what was observed in our study. We speculated a couple of reasons for our higher vaccine uptake than in the literature. First, our study participants were receiving regular nephrology care, where healthcare providers likely emphasized vaccination. Secondly, CRIC participants might have a stronger inclination toward healthy behaviors in general, as seen in their participation in a research study.

Factors significantly associated with influenza non-vaccination. (A) Demographic factors and social determinants of health. (B) Clinical conditions and health behaviors. Due to the number of characteristics examined in the analysis, the figure presents only those that showed significant associations. Figure 2 from Ishigami et al, © 2023, Elsevier.
AJKDBlog: Now looking at the vaccinated vs unvaccinated cohorts in CRIC – what characteristic differences did you observe?
Dr Ishigami: When comparing the two groups, the vaccinated cohort was more likely to be older, White, have diabetes, COPD, cancer, or ESKD, have higher education and household income, and be currently married. Characteristics such as sex, UPCR, functional health literacy, self-reported health-related quality of life, and smoking and drinking status were comparable between the two groups.
AJKDBlog: When you did multivariable analyses, what factors were associated with non-vaccination or infrequent vaccination?
Dr Ishigami: We found that younger age, Black race, lower educational attainment, lower annual household income, former marital status, and unemployed status were associated with a higher likelihood of non-influenza vaccination or infrequent vaccination. For instance, Black participants were 64% more likely to be in the non-vaccination status for influenza compared to White participants. Additionally, adverse social determinants of health were consistently associated with influenza non-vaccination.
Conversely, participants with several chronic conditions such as diabetes, COPD, and ESKD were more likely to receive an influenza vaccine. These diseases are recognized as high-risk conditions that increase the susceptibility to infections, potentially leading to increased awareness regarding the necessity of vaccination.
However, the presence of proteinuria was not associated with a higher likelihood of receiving an influenza vaccine, despite its independent association with infection. This finding is concerning. The underlying reasons are not fully clear, but it might indicate a lesser recognition of proteinuria as a risk factor for infection compared to low eGFR. Additionally, proteinuria is less frequently assessed than eGFR, resulting in fewer individuals being aware of having proteinuria.
AJKDBlog: When looking at this data, what should the nephrology community take away from this paper, and what can we do to increase vaccination uptake in high risk individuals and communities?
Dr Ishigami: Our data indicates there is still room for improvement in vaccine uptake among people with CKD. The Centers for Disease Control and Prevention’s Standards for Adult Immunization Practice emphasize that every clinical encounter with patients should be utilized to promote vaccination. However, while nephrology care providers acknowledge the advantages of influenza vaccination, some may not actively take on the responsibility of recommending the vaccination to their patients.
Nephrologists who have already established solid relationships with their patients may have a unique opportunity to increase vaccination rates in patients with CKD. Such efforts are particularly important for those who face barriers to vaccination (such as younger adults, Black individuals, and those with adverse social determinants of health). These factors are often clustered in communities due to structural inequities. Thus nephrology care providers should also involve community stakeholders (public agencies, caregivers, and patients) when developing vaccination programs. Such discussions can build mutual trust, delineate stakeholder needs, and provide supportive resources like educational materials and vaccine access.
To view Ishigami et al, please visit AJKD.org:
Title: Factors Associated With Non-vaccination for Influenza Among Patients With CKD: Findings From the Chronic Renal Insufficiency Cohort (CRIC) Study
Authors: Junichi Ishigami, Bernard G. Jaar, Jeanne B. Charleston, James P. Lash, Julia Brown, Jing Chen, Katherine T. Mills, Jonathan J. Taliercio, Sheru Kansal, Deidra C. Crews, Kristin A. Riekert, David W. Dowdy, Lawrence J. Appel, and Kunihiro Matsushita on behalf of theCRIC Study Investigators
DOI: 10.1053/j.ajkd.2023.06.007
We would like to invite blog post submissions related to next year’s World Kidney Day (WKD) campaign theme: “Kidney Health for All: Advancing equitable access to care and optimal medication practice”. Submissions should be between 800-1,200 words and sent to AJKD@pennmedicine.upenn.edu by February 14th, 2024.



Leave a Reply