#NephMadness 2024: Peritoneal Dialysis – Ah, Adequacy
Submit your picks! | NephMadness 2024 | #NephMadness
Jade Teakell @jmteakell
Dr. Jade Teakell is an Associate Professor of Medicine and the Associate Program Director for the Nephrology Fellowship at McGovern Medical School in Houston, TX. Her clinical and research interests are chronic kidney disease, home dialysis therapies, and reduction of health care disparities. She serves as the medical director for the Harris Health System Peritoneal Dialysis Program.
Competitors for the Peritoneal Dialysis Region
Team 1: PD First vs Team 2: Beyond Kt/V

Image generated by Evan Zeitler using Image Creator from Microsoft Designer, accessed via https://www.bing.com/images/create, January, 2024. After using the tool to generate the image, Zeitler and the NephMadness Executive Team reviewed and take full responsibility for the final graphic image.
It’s what one strives for in life, to be adequate. Every year in March, collegiate athletes pour blood, sweat, and tears into a frenzied competition to be crowned the nation’s most adequate basketball team. Not buying it? Why then is adequateness an acceptable target for life-sustaining dialysis therapy? Historically, adequacy in dialysis therapy has referred to Kt/V urea as a measure of small solute clearance. The Kt/V was derived using data from patients on hemodialysis (HD), and comprises the dialyzer clearance (K), the therapy time (t), and patients’ volume of distribution for urea (V). A simple, easily calculated figure to quantify dialysis dose is, of course, appealing for clinicians and regulators/payors alike. A target value of weekly Kt/V >1.7 was recommended for patients on peritoneal dialysis (PD) in 2006 guidelines by Kidney Disease Outcomes Quality Initiative (KDOQI) as well as the International Society for Peritoneal Dialysis (ISPD); in 2012 Centers for Medicare & Medicaid Services (CMS) incorporated this metric into their Quality Incentive Plan (QIP) making total weekly Kt/V urea >1.7 the sole measure for assessing dialysis quality of peritoneal dialysis (PD) in the United States.
Kt/V is imprecise to begin with, as estimating V can be difficult and assumptions must be made that sometimes result in indiscriminate substitutions of body weight, ideal body weight, adjusted body weight, and others. All formulas for V tend to overestimate the total body water for patients with obesity. In presuming a minimum necessary floor value for Kt/V exists, then preference or selection for patients with smaller V value can occur (implicitly or explicitly) which severely limits candidates in a country where adult obesity prevalence is >40%. Conversely, patients with smaller V could experience insufficient dialysis if Kt/V alone is used for assessment. Furthermore, current Kt/V measurement requirements for hemodialysis do not consider a patient’s residual kidney function (RKF) and thus do not require 24-hour urine collection and separate timed needlesticks that are required for patients on PD. So for patients on PD and facility staff, it is no longer a simple calculation from blood already accessed and parameters already measured.
But does Kt/V urea as a marker of dialysis quality really translate to PD? PD is inherently different.To quote the late Dr. Lysaght, “The peritoneum is not a simple barrier between two phases but rather a heterogeneous mucopolysaccharide hydrogel containing a labyrinthine vasculature through which blood flows as it equilibrates with a pool of dialysate residing within the peritoneal cavity.” In 1989 papers, Lysaght et al modeled dialysis mass transfer kinetics of peritoneal membranes and described the relationship of Kt/V for HD to continuous ambulatory peritoneal dialysis (CAPD). It is clear that mass transfer of urea per time is less for PD, but urea as a sole surrogate for all uremic solutes is an oversimplification. Importantly, compared to HD, the clearance of low molecular weight molecules is slower while that of middle‐molecules is higher. In the following two decades, three major studies – commonly referred to as CANUSA, ADAMEX, and Hong Kong Study – aimed to determine a Kt/V target for peritoneal dialysis that would improve survival. Findings from CANUSA (prospective, observational) initially set the target at >2.0, but a keen reanalysis of CANUSA in combination with findings from randomized controlled trials ADEMEX and Hong Kong resulted in the aforementioned target of >1.7 recommended by KDOQI/ISPD in 2006. In the past two decades since the Hong Kong Study, a limited number of observational studies have demonstrated that RKF is more important than small solute clearance and no clear survival benefit for the target weekly Kt/V >1.7. Very few studies have been done since 2008.
Notably, the major studies on which the Kt/V >1.7 target was based were performed in patient populations exclusively using CAPD (manual exchanges, continuous therapy). The United States has a very low rate of CAPD utilization, with the USRDS 2023 Annual Data Report showing 88% of prevalent patients on PD are using APD (cycler exchanges, and not always continuous therapy). Adequacy in APD has not actually been defined precisely, though mathematical modeling shows a CAPD-equivalent weekly Kt/V that can be calculated. This was the case in the 1997 KDOQI guidelines where a higher Kt/V target for patients on continuous cycling PD (CCPD) or APD with no daytime dwell (dry day), was “in the absence of data, recommended based on theoretical considerations.” In the 2006 guidelines, KDOQI go on to state that “in view of the very limited data about APD clearances and outcomes, no guidelines are possible for small-molecule clearance on APD therapy.” Yet in the ADP-loving United States, many have held fast to this metric target that not only has fallen out of favor with international guidelines but may actually be flawed for the PD modality preferred by many patients.
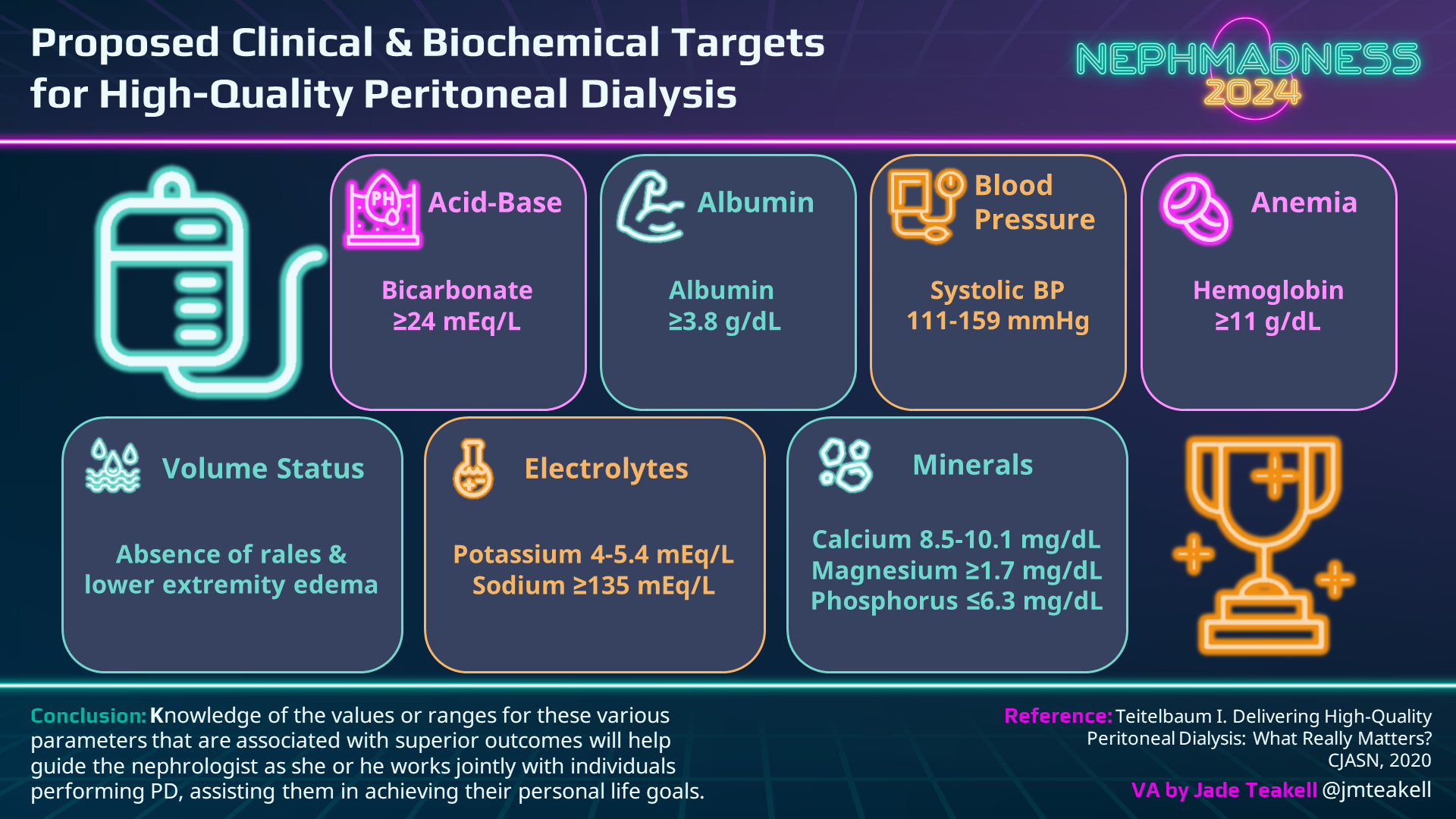
In 2020, the ISPD published their practice recommendations for prescribing peritoneal dialysis. In this updated version, authors acknowledge that there is no high-quality evidence to support the attainment of a specific Kt/V target previously recommended. The KDOQI workgroup essentially agreed in their 2021 commentary. Both groups recommend to decrease emphasis on a specific target for small solute clearance, and to instead focus on a more holistic assessment of metabolic and volume status as well as quality of life. Despite the underwhelming data to support Kt/V and calls for change from home dialysis leaders, current US federal regulations keep the status quo. Maliha and colleagues have outlined a path forward for the United States in a recent JASN perspective. They describe a 3-step approach whereby CMS could acknowledge international guidelines, change the Kt/V from a clinical measure of quality (which affects facility reimbursement via QIP) to simply a reportable measure, and establish a defined billing code (or modifier) that would identify patients on an alternative pathway. Importantly, this approach would allow for outcome comparison for patients in the United States following the traditional (Kt/V >1.7) versus alternative (2020 ISPD guidelines), and it could allow for expansion of peritoneal dialysis uptake and reduce peritoneal dialysis attrition. There are several measurable biometrics that could as well as patient-centered quality of life metrics that could replace the Kt/V for clinicians and CMS to ensure quality.
People are of all shapes and sizes, and they have myriad life plans and goals. Why should one calculated, urea-centric value define what is “adequate” for them all? If a patient has chosen home peritoneal dialysis therapy, we should not accept “adequate.” We should aim to provide “high-quality, goal-directed,” patient-centric peritoneal dialysis therapy.
“Good enough is not good enough.” -Stephen Curry
Good luck, Team Beyond Kt/V, I’m cheering for you!

Copyright: Canities/Shutterstock
– Guest Post written by Jade Teakell @jmteakell
As with all content on the AJKD Blog, the opinions expressed are those of the author of each post and are not necessarily shared or endorsed by the AJKD Blog, AJKD, the National Kidney Foundation, Elsevier, or any other entity unless explicitly stated.
Click to read the Peritoneal Dialysis Region
Submit your picks! | #NephMadness | @NephMadness


Leave a Reply