PD or HD: Which One Gets a Higher Readmisssion Score?

Copyright: icetray / 123RF Stock Photo
The utilization of peritoneal dialysis (PD) in the United States certainly lags behind other countries. As a result, our view of 30-day hospital readmission rates with respect to in-center hemodialysis (ICHD) patients may be skewed compared to that of peritoneal dialysis (PD) patients. In a recent AJKD article, Perl et al examine the end-stage renal disease (ESRD) population in Canada, which has high rates of PD use.
The authors evaluated a matched cohort of 8,026 patients on ICHD and 4,013 patients on PD. They found that the 30-day readmission rates were 7.1 per 1,000 person-days for patients on PD and 6.0 per 1,000 person-days for patients on ICHD. Interestingly, approximately 80% of re-hospitalizations in their cohort were for reasons different from those responsible for the index hospitalization.
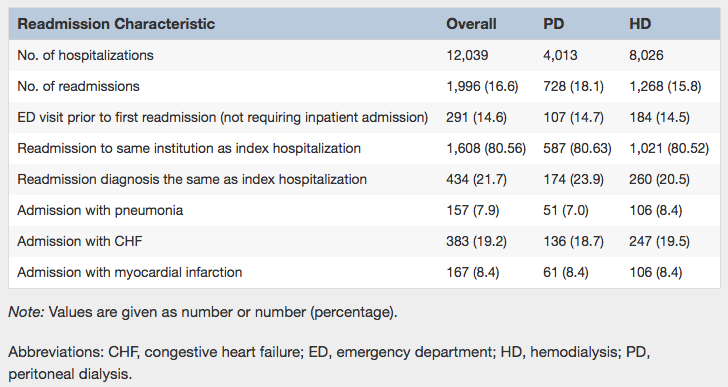
Table 3 from Perl et al, AJKD, © National Kidney Foundation.
If applicable in other geographic settings and patient cohorts, the results of this study raise the question of the economic benefit of PD as well as the perceived mortality equivalence to ICHD. The main issue raised by the authors concerns post-discharge follow-up. ICHD patients are evaluated during their scheduled hemodialysis session, which likely falls within 1-2 days post discharge. On the other hand, PD patients may experience delays in follow-up post discharge, as their evaluations tend to occur on a monthly rather than weekly basis.
According to the United States Renal Data System (USRDS), in 2014 88.1% of all incident cases began renal replacement therapy with hemodialysis and 9.3% started with PD. While there is a drastic difference between ICHD and PD use in the United States, one major trend is the continued—albeit small—increase in PD use. As PD use grows in the United States, we must be mindful of the post-discharge phenomenon highlighted in this study. Protocols for post-discharge evaluation (e.g., medication reconciliation, novel access issues, and hospital-acquired infections) should be put in place so as to prevent readmissions for separate reasons. The authors emphasize that future studies are needed regarding patient, provider, and systems issues that lead to readmissions among dialysis patients.
Post prepared by Sean Kalloo, AJKD Blog Contributor
To view the Perl et al article abstract or full-text (subscription required), please visit AJKD.org.

Leave a Reply