Cystatin-C and Cr-Based eGFRs: What Differences Does the Difference Make?
AJKDBlog Interviews Editor Timothy Yau (@Maximal_Change) caught up with Juan-Jesús Carrero (@jjcarrero1) and Edouard Fu (@FuEdouard) to chat about their research recently published in AJKD on discrepancies between estimated glomerular filtration rate (eGFR) based on creatinine (eGFRcr) and based on cystatin C (eGFRcys), and how cystatin C testing in Sweden can shed a light on this.
Juan Jesus Carrero is Professor of Kidney Epidemiology at Karolinska Institutet. His main areas of research involve modifiable risk factors for CKD: diet/lifestyle, healthcare gaps and inappropriate use of medications.
Edouard Fu’s research focusses on studying medication effectiveness and safety using routinely collected healthcare data and causal inference methods, as well as optimal estimation of kidney function.
AJKDBlog: Let’s start with the basics. Most of our readers are familiar with serum creatinine (SCr) and the pitfalls/problems (age, muscle mass, etc) when using this to estimate GFR. What is cystatin C and can you point out some of the issues that may lead to inaccurate GFR estimations?
Drs Carrero and Fu: It is difficult to measure GFR, and instead it is often estimated by using the concentrations of endogenous filtration markers. Besides glomerular filtration rate, the concentration of filtration markers are affected by generation, tubular reabsorption, secretion and extrarenal elimination. For instance, creatinine is influenced by muscle mass, diet, physical activity, and certain drugs.
Cystatin C is an alternative filtration marker that can be used for GFR estimation. It is produced by all nucleated cells, freely filtered by the glomerulus, and metabolized in the tubules, so it is not excreted in the urine. Whenever eGFRcr is thought be inaccurate, it is recommended to perform a second-line or confirmatory test, e.g. with eGFR based on cystatin C (eGFRcys). However, it is important to note that there are also non-GFR determinants of cystatin C, such as obesity, smoking and inflammation.
Previous studies have shown that eGFRcys is not more accurate than eGFRcr; combining creatinine and cystatin C to estimate GFR best approximates kidney function. This is likely due to the fact that combining both markers reduces errors that are due to variation in the non-GFR determinants of each marker.
AJKDBlog: Despite many clinical guidelines recommending its use, cystatin C has not made its way into regular routine use in the US. Can you outline how it has been used in Sweden over the past years and how researchers like Anders Grubb have impacted its use in clinical practice?
Drs Carrero and Fu: Indeed, routine cystatin C testing has been available for over a decade in Sweden. In 1985, Swedish physician Dr. Anders Grubb proposed cystatin C as a filtration marker. He led landmark research in this area and was instrumental to its widespread use in our country.
Cystatin C is routinely measured in Swedish Healthcare, often as part of the kidney function evaluation package (together with creatinine and albuminuria). However, cystatin C testing is not Universal: In the population of Stockholm (Sweden), we found that around 11% of patients with a creatinine test also receive a cystatin C test, with an annual rate of cystatin C testing between 4-7%. Cystatin C is more likely to be tested in those who are older, have a lower eGFRcr and more comorbid conditions. When cystatin C is ordered in routine care, Swedish clinicians receive an automatic reporting of eGFRcys, eGFRcr and the average between eGFRcys and eGFRcr.
When eGFRcr and eGFRcys agree (e.g. within 20% of each other), then their average is recommended. If they do not agree, then non-renal factors need to be assessed which influence eGFRcys or eGFRcr, and one must determine which one is most accurate.
AJKDBlog: Your paper brings up a concept called the eGFRdiffcys-cr. You define this as the difference in eGFR when using cystatin C-based eGFR and creatinine-based eGFR. What were the outcomes you looked at when exploring this index and why did you choose these?
Drs Carrero and Fu: Cystatin C–based eGFR (eGFRcys) and creatinine-based eGFR (eGFRcr) measured in the same individual may be different due to differences in non-GFR factors affecting their serum concentrations. We were interested in finding out whether a large eGFRdiff was common in routine clinical practice and what the impact of these differences was on prognosis. Specifically, we looked at the outcomes kidney failure with replacement therapy (KFRT), acute kidney injury (AKI), heart failure, atherosclerotic cardiovascular disease (composite of myocardial infarction and stroke), all-cause death, and cardiovascular death. These outcomes have previously been shown to be associated with eGFR, and are common adverse events in people with CKD.
AJKDBlog: Before we look at the results, can you tell us what you found when looking at the eGFRs based on creatinine and cystatin-C? There appears to be considerable discordance between the values with eGFRcys generally lower than eGFRcr
Drs Carrero and Fu: In total, we included 158,601 individuals who had simultaneous creatinine and cystatin C tests. We found that on average, eGFRcys was lower than eGFRcr within the same individual. Around one third (32%) had a difference of more than 15 mL/min/1.73 m2. This contrasts with the smaller discordances found in research cohorts such as the CRIC or SPRINT trial. Patients with larger negative eGFRdiffcys-cr (eGFRcys<eGFRcr) were older, more often female, with higher eGFRcr and albuminuria, and more comorbid conditions.
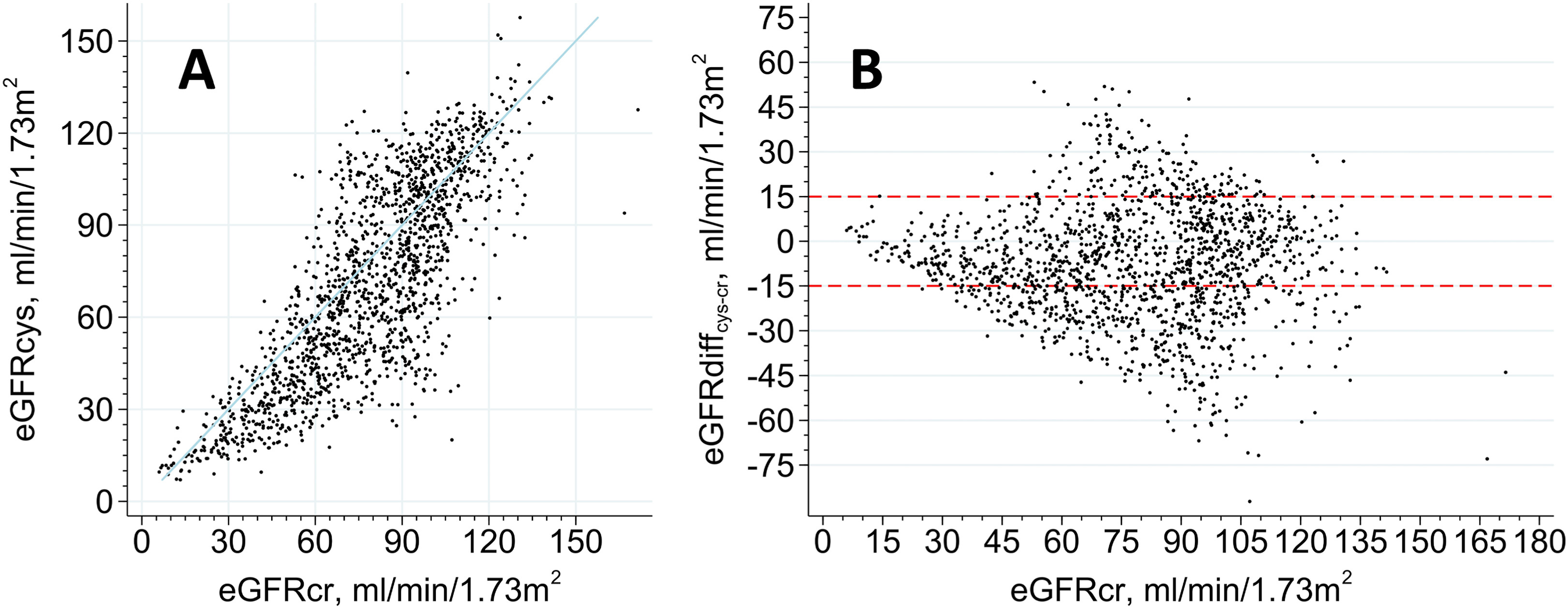
(A) Univariate correlation between eGFRcys and eGFRcr, and (B) scatterplot of eGFRcr versus eGFRdiff at baseline. Shown are correlations in a random 1% sample of 1,569 observations. The blue line shows the line of identity, and red line marks eGFRdiff higher and lower than 15 mL/min/1.73 m2. Figure 1 from Carrero et al, © 2023, the authors.
AJKDBlog: What were the big takeaway findings when looking at the outcomes like death, cardiac events, and kidney events?
Drs Carrero and Fu: Compared to patients with similar eGFRcys and eGFRcr, a larger negative eGFRdiffcys-cr (eGFRcys< eGFRcr) was associated with a higher adjusted hazard ratio for all study outcomes. The lower the eGFRcys compared with eGFRcr, the higher the hazards for all outcomes. We found that a negative 15 mL/min/1.73 m2 difference was associated with a two fold increased risk for all outcomes.

Adjusted Hazard Ratios for Outcomes Associated With Quartiles of eGFRdiff. Table 2 from Carrero et al, © 2023, the authors.
AJKDBlog: What are some possible explanations for the large differences between the eGFRs estimated from cystatin-C and creatinine? And how do your findings from this paper impact clinical practice?
Drs Carrero and Fu: We believe that eGFRdiff may represent the risks attributed to the non-GFR determinants of creatinine and cystatin C. Older age and poor health status tend to result in lower creatinine for the same level of GFR, likely due to low muscle mass, whereas cystatin C can be elevated for the same level of GFR in the setting of chronic inflammation. As shown in our study, eGFRdiff were more negative at higher eGFRcr values, which may reflect the capture of frail individuals with inappropriately low serum creatinine. Such frail individuals may have a poorer prognosis. An alternative explanation proposed by others is that large eGFRdiff reflects selective impairment of glomerular sieving of cystatin C and other middle molecular weight macromolecules as an early manifestation of CKD. However, we are not aware of studies demonstrating this glomerular sieving yet.
The clinical implications of our study are that many patients have discordance eGFRcys and eGFRcr in routine clinical practice, and assessing their discordance can be useful for risk stratification, monitoring health status, and prompting clinical actions. This will become more important as cystatin C measurements make more headway into everyday clinical practice.
To view Carrero et al (Open Access), please visit AJKD.org:
Title: Discordances Between Creatinine- and Cystatin C–Based Estimated GFR and Adverse Clinical Outcomes in Routine Clinical Practice
Authors: Juan-Jesús Carrero, Edouard L. Fu, Yingying Sang, Shoshana Ballew, Marie Evans, Carl-Gustaf Elinder, Peter Barany, Lesley A. Inker, Andrew S. Levey, Josef Coresh, and Morgan E. Grams
DOI: 10.1053/j.ajkd.2023.04.002
We would like to invite blog post submissions related to next year’s World Kidney Day (WKD) campaign theme: “Kidney Health for All: Advancing equitable access to care and optimal medication practice”. Submissions should be between 800-1,200 words and sent to AJKD@pennmedicine.upenn.edu by February 14th, 2024.



Leave a Reply