Urea for the Treatment of Hyponatremia 2/2 SIADH: An Interview
The use of urea to treat hyponatremia related to the syndrome of inappropriate antidiuretic hormone secretion (SIADH) has not been universally adopted due to questions about effectiveness, safety, and tolerability. In a systematic review and meta-analysis recently published in AJKD, Chander and colleagues used observational studies to address these questions.
AJKDBlog Interviews Editor Timothy Yau (@Maximal_Change) caught up with Dr. Chander to discuss if urea is effective for managing SIADH-induced hyponatremia.
Dr. Subhash Chander (@DeewanSubhash) is a nephrologist currently completing his Critical Care Medicine fellowship at Mayo Clinic in Rochester, Minnesota, where he is combining his expertise in nephrology with advanced training in critical care. His clinical and research interests focus on electrolyte imbalances, kidney disease, and the management of critically ill patients, particularly those requiring renal replacement therapy and ECMO support.
AJKD Blog: Before we get into the study itself, I think a little background on urea and SIADH would be nice to set the stage. If you were giving a lecture to nephrology fellow trainees, how would you explain how urea treats hyponatremia in SIADH from a physiologic standpoint?
Dr. Chander: Hyponatremia is primarily a disorder of water balance rather than a direct sodium deficit. In SIADH, excessive ADH secretion leads to inappropriate water retention through activation of V2 receptors in the renal collecting ducts, resulting in dilutional hyponatremia. This excess water retention lowers plasma osmolality and suppresses sodium concentration without an actual sodium deficit.
Urea is an effective treatment for SIADH because it increases renal solute excretion, thereby enhancing free water clearance. Unlike sodium-based therapies such as hypertonic saline, salt tablets, and loop diuretics, urea does not rely on sodium retention or volume expansion to achieve its effect. Instead, it acts as an osmotic agent that is freely filtered by the kidneys and partially reabsorbed in the collecting ducts. This increases urine osmolality and promotes water excretion without causing excessive sodium loss.
By augmenting renal solute load, urea facilitates a gradual and controlled correction of hyponatremia while reducing the risk of overcorrection or volume overload. Its cost-effectiveness and availability make it particularly useful in resource-limited settings, and its favorable safety profile makes it a practical option for both acute and long-term management of SIADH.
AJKD Blog: Piggybacking off the last question – what is different about urea compared to simply increasing sodium intake, or using salt tabs to help increase solute load to achieve the same purpose of raising osmolality?
Dr. Chander: This is a particularly interesting point that many nephrologists have yet to fully recognize. The key distinction between urea and sodium-based therapies, such as salt tablets or increased sodium intake, lies in their mechanisms of action on water excretion and therefore sodium balance. Urea enhances free water excretion without increasing sodium retention. As a non-sodium osmotic agent, it increases renal solute load, thereby promoting water excretion and reducing dilutional hyponatremia independently of sodium levels. This makes urea especially beneficial for patients at risk of volume overload, such as those with heart failure or cirrhosis.
In contrast, salt tablets and increased sodium intake work by increasing serum osmolality to promote water excretion, but their effectiveness depends on the kidney’s ability to excrete excess sodium in the collecting tubules. This mechanism may be less reliable in patients with SIADH, where inappropriate ADH secretion leads to persistent water retention despite increased sodium intake.
Furthermore, our meta-analysis demonstrated that urea is more effective in correcting hyponatremia while causing fewer adverse effects compared to salt tablets. It offers a safer, more cost-effective, and efficient approach to increasing solute load and enhancing free water excretion without significantly altering sodium balance. Its superior tolerability and efficacy make it an optimal treatment option for SIADH, particularly in patients who cannot tolerate sodium-based therapies or who are at risk of volume overload.
AJKD Blog: Now onto the study – this was a meta-analysis of studies using urea in hyponatremia. What kinds of studies were included in your analysis?
Dr. Chander: We searched four major electronic databases− PubMed/MEDLINE, EMBASE, Google Scholar, and Cochrane − to identify relevant studies. After applying the set inclusion criteria, a total of 16 studies were included, including 518 patients who received urea therapy. The selection criteria focused on clinical trials and observational studies reporting outcomes related to correction of serum sodium level, symptom resolution, or adverse effects. However, no RCTs were identified for inclusion.
The included studies investigated different doses of urea, ranging from 7.5g to 90g per day, administered either orally or via a nasogastric tube. Most studies reported serum sodium concentration as the primary outcome, while some also assessed urine osmolality, treatment duration, and patient tolerability. A subgroup of studies compared urea with other treatment modalities, including fluid restriction, vaptans, and no treatment, providing insight into its comparative effectiveness.
To illustrate our study selection process, Figure 1 presents a PRISMA flow diagram detailing the identification, screening, and inclusion of studies in this meta-analysis.
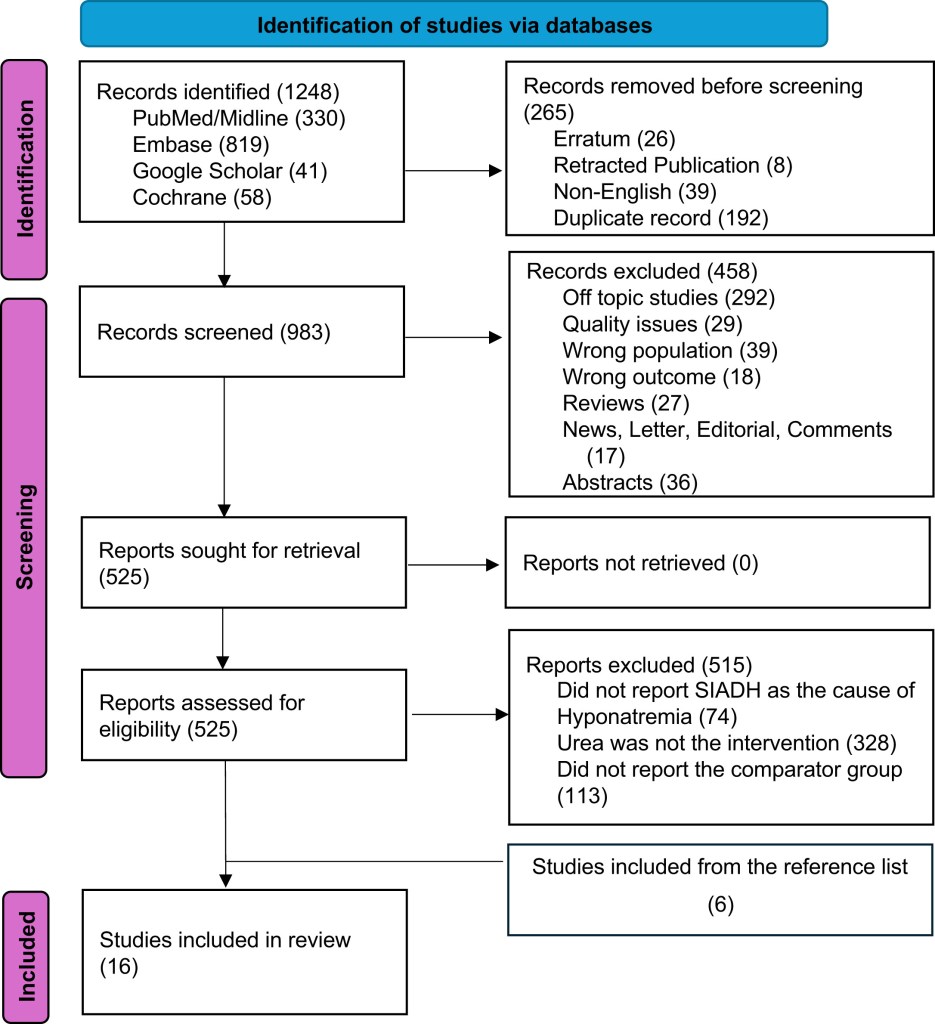
PRISMA flow chart. Figure 1 from Chander et al, © National Kidney Foundation.
AJKD Blog: What were some of the data points you looked at in the analysis? I am particularly interested in the serum Na concentration and urine osmolarity, in addition to the response to different doses and durations of oral urea.
Dr. Chander: An analysis of data from 16 studies demonstrated that urea treatment significantly increased serum sodium levels in patients with SIADH, with a mean difference (MD) of 9.21 mEq/L (95% CI: 7.36-11.06, P < 0.01).
Subgroup analysis based on treatment duration revealed a significant rise in serum sodium at various time points. After 24 hours, the increase was MD 3.57 mEq/L (95% CI: 2.51-4.62). The sodium correction continued over 2 days (MD 8.16, 95% CI: 4.98-11.34), 3 days (MD 7.92, 95% CI: 6.56-9.28), and 5 days (MD 7.73, 95% CI: 4.54-10.91). By 7 days, the sodium increase was MD 14.66 (95% CI: 2.71-26.61). At 14 days, the effect was MD 8.34 (95% CI: 7.04-9.63), and at 1 year, it remained stable at MD 9.48 (95% CI: 8.09-10.86), demonstrating the sustained efficacy of urea therapy over time.
A subgroup analysis indicated a severity-dependent effect, with greater improvements observed in patients with severe hyponatremia (<120 mEq/L), where the increase was MD 18.04 mEq/L (95% CI: 13.68-22.39). In comparison, patients with moderate SIADH (120-129 mEq/L) experienced a smaller increase (MD 7.87, 95% CI: 6.76-8.99), and those with mild SIADH (130-135 mEq/L) had a similar response (MD 8.00, 95% CI: 7.31-8.69).
These findings highlight urea’s effectiveness across different severities and treatment durations, making it a viable long-term therapeutic option for SIADH.
AJKD Blog: What were some of the big takeaways you found when looking across the studies? And were there any adverse or safety events that impacted the general tolerability of urea?
Dr. Chander: Urea has been shown to be an effective treatment for correcting serum sodium levels in patients with SIADH, demonstrating a dose-dependent response, with more severe hyponatremia showing greater improvement. Its effects are sustained over both short- and long-term treatment periods, with sodium level improvements observed even after one year of therapy.
In terms of safety, urea is generally well-tolerated, and the most frequently reported adverse event associated with treatment was poor palatability, affecting 17-54% of patients across various studies. Hypernatremia occurred in 8-14% of cases, though it was neither severe nor clinically significant. Gastrointestinal symptoms, such as nausea and reflux, were rare and generally mild. Notably, no cases of osmotic demyelination syndrome (ODS) were reported, further reinforcing the safety of urea therapy.
Some patients discontinued treatment due to its unpleasant taste rather than experiencing significant side effects. Overall, urea demonstrated a favorable safety profile and was well-tolerated compared to other treatment options for SIADH, making it a viable alternative in clinical practice.
AJKD Blog: How do the findings from this meta-analysis impact a clinician’s bedside decision-making process when it comes to treating a challenging disorder like SIADH? Closing thoughts?
Dr. Chander: The findings demonstrate that urea is an effective, safe, and cost-efficient treatment for SIADH. Clinicians can consider oral urea as a first- or second-line therapy, particularly in cases where fluid restriction is poorly tolerated or impractical, or in patients requiring close monitoring due to conditions such as heart failure or cirrhosis, where rapid sodium correction is not required, and long-term management is necessary to maintain sodium balance.
It also serves as a practical option for sustained sodium correction. Clinicians should educate patients about taste-related concerns and explore strategies such as mixing urea with sweeteners to improve palatability. Additionally, regular monitoring for hypernatremia and adherence is essential, with dosing adjustments tailored to the severity of SIADH to optimize treatment outcomes.
These findings support the broader integration of urea into clinical practice, particularly in resource-limited settings, where cost-effective and accessible treatment options play a crucial role in the effective management of hyponatremia.
To view Chander et al [Subscription Required], please visit AJKD.org.
Title: Urea to Treat Hyponatremia Due to Syndrome of Inappropriate Antidiuretic Hormone Secretion: A Systematic Review and Meta-Analysis
Authors: Subhash Chander, Roopa Kumari, Abhi Chand Lohana, Zubair Rahaman, Om Parkash, Sheena Shiwlani, Yaqub Nadeem Mohammed, Hong Yu Wang, Hao Chi, Wenchy Tan, Sanjay Kirshan Kumar, FNU Sindhu
DOI: 10.1053/j.ajkd.2024.07.011

Leave a Reply