Acute and Chronic Antibody-Mediated Rejection Represent a Continuum of Endothelial Injury Involving Multiple Immune Mechanisms
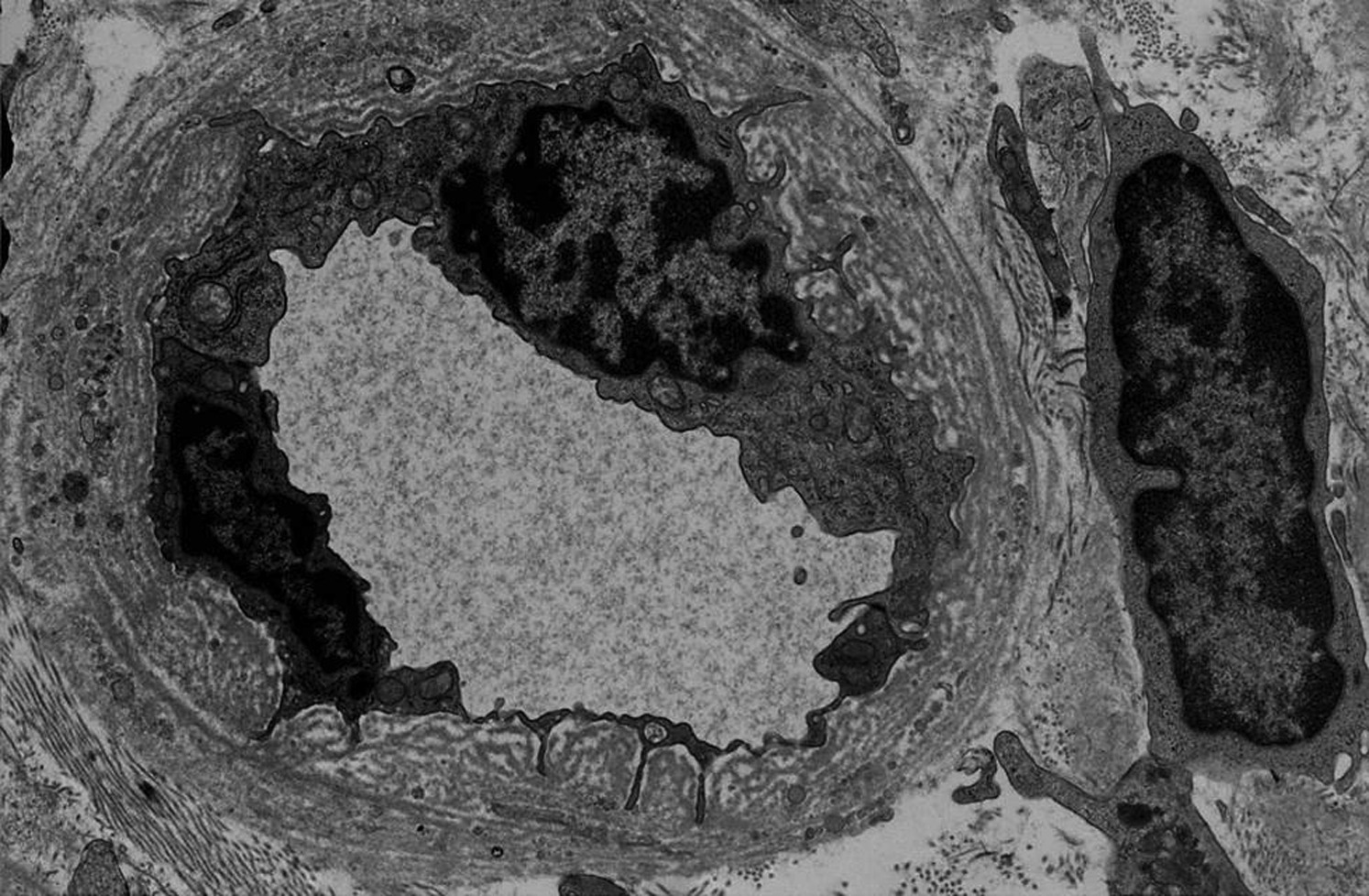
Fig 3 Najafian et al AJKD, © National Kidney Foundation.
A comparison of the criteria for acute and chronic antibody-mediated rejection (ABMR) in the November installment of the AJKD Atlas of Renal Pathology II shows that only criterion 1, which refers to histologic evidence of chronic tissue injury, is unique. Evidence for current/recent histologic interaction of antibody interaction with endothelium (criterion 2) and presence of donor specific antibodies (criterion 3) are common in both conditions. Chronic transplant glomerulopathy, defined as duplication of glomerular basement membranes is essentially the aftermath of glomerulitis, which is used to define acute ABMR. Multilayering of peritubular capillary basement membranes is an analogous lesion that results from persistent peritubular capillaritis (ptc). Along the same lines, new onset arterial intimal fibrosis is the result of damage to the arterial intima in the acute phase of antibody-mediated injury.
Immunohistochemistry studies show that about 30% of the cells in glomerulitis lesions are T-cells (mostly CD8 positive T-cytotoxic cells), while the remaining are macrophages. Macrophages may have both an antigen processing and scavenging function. Likewise, arterial lesions seen in the context of ABMR have a significant number of T-cells infiltrating the arterial intima. A small number of NK cells is also present and suggests that antibody dependent cytotoxicity is an additional mechanism of tissue injury. Thus, the cellular immune system (T-cells) and innate immunity (NK cells) contribute to graft loss that is commonly interpreted simply as chronic ABMR (Sellares et al, Halloran et al). I believe that the emphasis only on ABMR as a cause of late graft failure is not conducive to the development of optimal therapies for chronic rejection. Chronic rejection remains and important unsolved problem in the field of kidney transplantation, and its prevention/treatment will require recognition and mitigation of the concurrent deleterious action of T-cells, NK-cells, and macrophages (Randhawa).
Dr. Parmjeet Randhawa
AJKD Blog Contributor and AJKD Associate Editor
Please visit the Atlas of Renal Pathology II at AJKD.org to view the related installments on acute and chronic ABMR (freely available).

Leave a Reply